The effect of Hepatitis B Virus Infection on Long-Term Outcomes after Kidney Transplantation
*Qing Yuan1,2,3, *Shanjuan Hong1, *Eve Roth1,3, *Andric Perez-Ortiz1, Nahel Elias1,3
1Massachusetts General Hospital, Boston, MA;28th Medical Center, Chinese PLA General Hospital, Beijing, China3Harvard Medical School, Boston, MA
Objective: To investigate the effects of Hepatitis B Virus (HBV) infection in kidney recipients and donors on long-term post-transplant outcomes.
Design: Propensity score matched analysis of a retrospective cohort study from the Organ Procurement and Transplantation Network (OPTN) as of June 2019.
Setting: National database of all kidney transplants in the US.
Patients: Adult recipients of solitary kidney transplants from ABO-compatible deceased donors between January 2000 and March 2019. We identified three cohorts based on donor and recipient HBV surface antigen (HBsAg) status: D-R-, D-R+, D+R-.
Main Outcome Measures: Patient survival (PS) and death-censored graft survival (DCGS).
Results: From 2000 to 2019, 169,627 D-R-, 3,504 D-R+ and 127 D+R- patients underwent transplant. In the D+R- cohorts, 96 recipients were HBcAb-, 21 HBcAb+ and 10 HBcAb unknown. D+R- donors were younger than D-R- (34.5±15.9 vs. 38.6±15.7, p=0.003), more likely HCV co-infected (5.5% vs. 3.2%, p=0.007), with longer cold ischemia time (19.7±7.4 h vs. 18.0±8.8 h, p=0.034);and D+R- recipients were more African American (39.4% vs. 32.5%, p=0.011), with lower panel reactive antibodies (12.9±28.7 vs. 19.8±33.8, p= 0.026). We found comparable PS and DCGS between D+R- and D-R-, and between D-R- and D-R+. There was no statistically significant difference between donor’s HBV infection and recipient’s HBV infection on the PS or DCGS posttransplant (Figure).
Conclusions: HBV infection in donors or recipient was not a risk factor affecting patient or graft survival. With appropriate management, broader utilization of HBV+ kidneys as well as kidney transplant in HBV+ recipients could be advocated, especially in endemic areas. 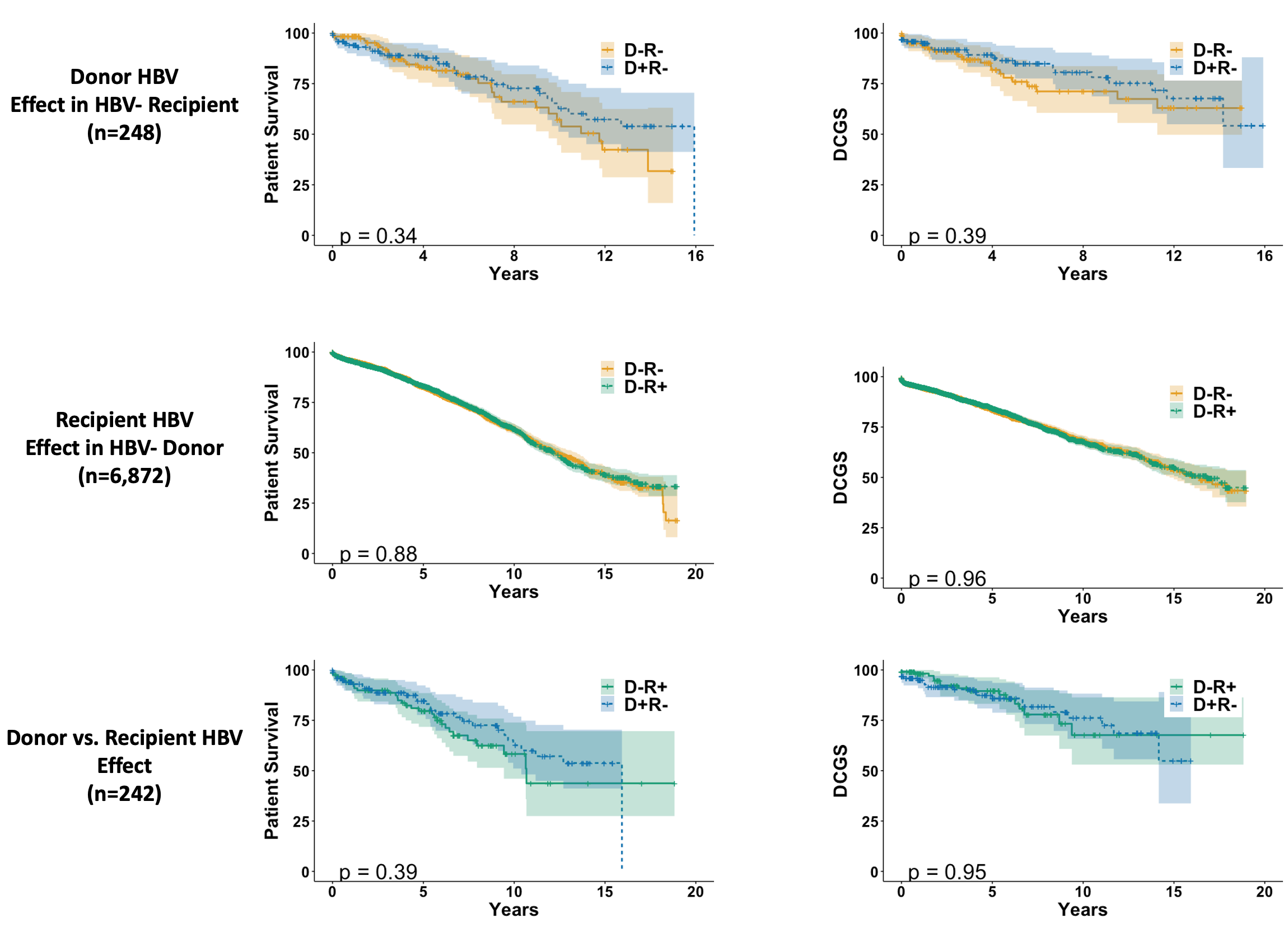
Back to 2020 Abstracts
