Thoracic Robot Emergency Scenario Simulations: How to Feasibly Teach Them
Kevin M. Dickson1, Bryce M. Bludevich1, Chelsea Jeewoo Lim1, Max D. Hazeltine1, Hannah Buettner1, Anne Weaver2, Jorge Yarzebski2, Isabel Emmerick1, Maksim Zayaruzny3, Mark Maxfield1, Mamatha Kadiyala3, Karl Uy1, Feiran Lou1
1Department of Surgery, UMASS Medical School, Worcester, Massachusetts, United States, 2Department of Simulation, UMASS TH Chan Medical School, Worcester, Massachusetts, United States, 3Department of Anesthesia, UMASS TH Chan Medical School, Worcester, Massachusetts, United States
Objectives: Although robotic surgery has gained popularity in the recent years, some thoracic surgeons have been hesitant to adopt this approach. One of the concerns is the potential delay in addressing intraoperative catastrophic hemorrhages since the surgeon is not at bedside. This study aimed to create a simulation-based educational system to teach emergent undocking skills to thoracic operating room (OR) teams.
Design: The first phase of this study focused on creation of a thoracic emergency undocking protocol and checklists for emergency scenarios through in-situ OR simulations of five specific situations, including massive hemorrhage from the pulmonary artery leading to hemodynamic instability. In the second phase of this study, the protocol and checklists were introduced to different OR teams by either: high-fidelity simulation or video-based didactic sessions.
Setting: The simulations were performed in a fully functional OR and the video-based didactic sessions were provided electronically.
Patients: There were no patients involved in this study.
Interventions: Two different OR teams participated in each learning method.
Main outcome measures: The performances of OR teams were tested with in-situ OR simulations of the same five scenarios. Assessments of effectiveness were done by comparing participants from phases I and II. Measurements included participant-reported feedback, timeliness of crucial conversion steps, and the number of missed critical steps.
Results: All teams were able to successfully convert from robot-assisted to open, with the attending being scrubbed and at bedside within five minutes from the decision to convert, regardless of phase or education type. Teams in phase I had more critical misses in the protocol and checklists than did teams in phase II. Phase I teams completed an average of 23/25 critical checklist points, while phase II teams completed an average of 25/25 critical checklist points. Following the final in-situ simulation, 97% of participants agreed that they confidently knew their role during an intra-operative emergency compared to 83% prior to any education or simulation. Most team members (94%) agreed that emergency checklists are helpful following their final simulation session. 89% of participants rated the quality of the checklists as either "excellent" or "above average." When comparing phases I and II, there was no significant difference in the time required for the attending to be present at the bedside, which averaged approximately 132 seconds.
Conclusion: Emergency checklists and protocols help teams remember crucial actions and also serve as a reference during high-stakes, low-frequency events. Targeted education regarding these crucial scenarios can lead to improved protocol adherence and help prevent critical misses. This study shows that high-fidelity simulation and didactic sessions can both be used to effectively teach emergency undocking protocols.
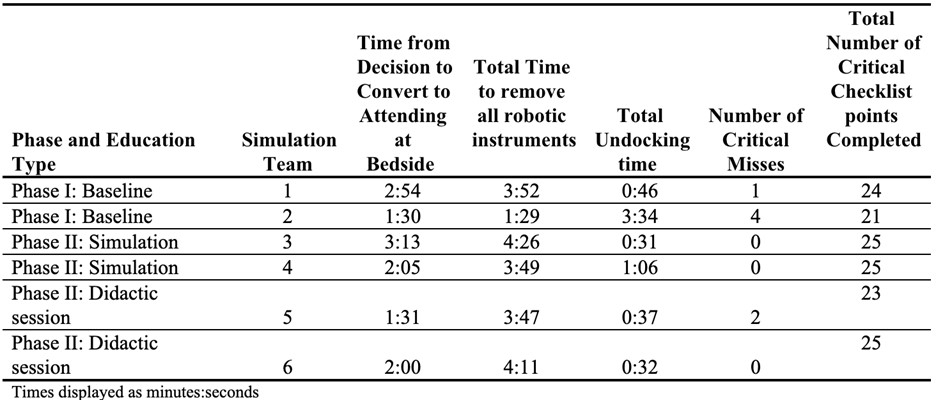
Title: Quantitative measures of completion of emergency checklists and protocol during both study phases.
Back to 2022 Abstracts
