Direct Thrombin Inhibitors as Alternatives to Heparin to Preserve Lung Growth and Function in Congenital Diaphragmatic Hernia
Savas T. Tsikis, Thomas Hirsch, Scott C. Fligor, Amy Pan, Malachi M. Joiner, Paul Mitchell, Kathleen M. Gura, Mark Puder
Vascular Biology Program, Department of Surgery, Boston Children's Hospital, Boston, Massachusetts, United States
OBJECTIVE
Infants born with congenital diaphragmatic hernia (CDH) frequently require cardiopulmonary bypass through extracorporeal membrane oxygenation (ECMO) and systemic anticoagulation. Heparin is the most common choice of anticoagulant used in this setting. Expeditious lung growth while on ECMO is necessary to improve the up to 50% mortality observed in CDH. We have previously demonstrated that heparin impairs both lung growth and angiogenic signaling in a murine model of compensatory lung growth (CLG) following left pneumonectomy. We investigate the pulmonary and molecular effects of the direct thrombin inhibitors (DTIs) bivalirudin and argatroban in this model.
DESIGN
Male C57BL/6J mice underwent left pneumonectomy and subcutaneous implantation of osmotic pumps. Pumps were pre-loaded with normal saline (control), bivalirudin, argatroban, or heparin at established dosages to achieve therapeutic systemic anticoagulation. On postoperative day 8, mice underwent pulmonary function testing (PFT), lung volume measurement, treadmill exercise tolerance testing (TETT), and lung protein analysis.
SETTING
Laboratory
PARTICIPANTS
7 to 8-week-old C57BL/6J mice
INTERVENTIONS
Left pneumonectomy followed by continuous administration of anticoagulants:
Bivalirudin: 50 μg/hr
Argatroban: 50 μg/hr
Heparin: 2.5 IU/hr
MAIN OUTCOME MEASURES
PFT: Total Lung Capacity (TLC)
Lung volume measurement
TETT: percent change from baseline in distance run and running time
Lung protein expression of angiogenic targets: Vascular endothelial growth factor (VEGF), VEGF receptor 2 (VEGFR2), activated phosphorylated VEGFR2 (pVEGFR2)
RESULTS
Initial dose-response studies determined the dosing needed for each anticoagulant to achieve therapeutic anticoagulation (data not shown).
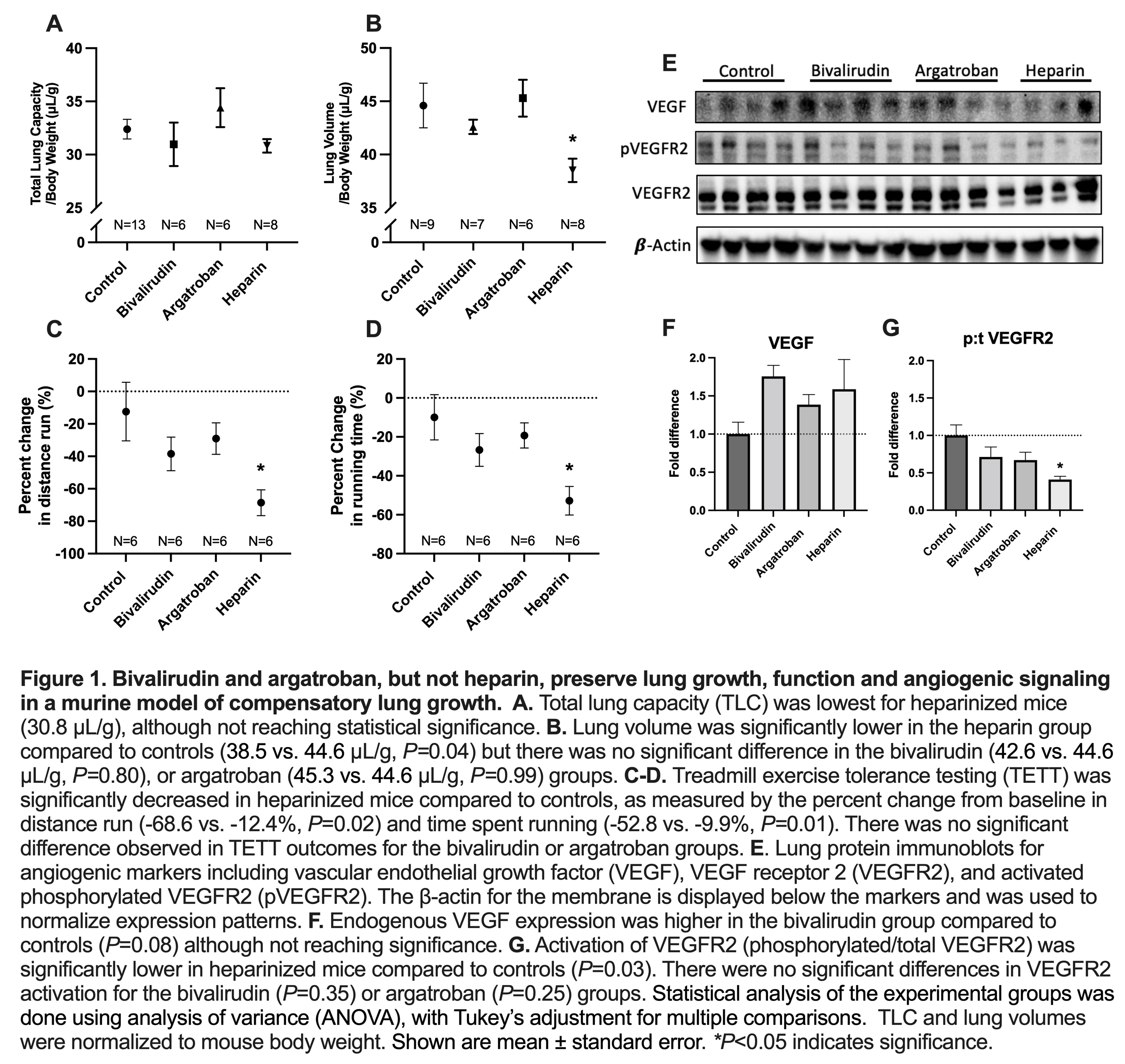
Heparin administration decreased lung volume (P=0.04) compared to control. TLC was lowest for heparinized mice, although not reaching statistical significance. Bivalirudin/argatroban did not significantly alter lung volume or TLC.
Heparin decreased TETT compared to control as measured by the percent change from baseline in distance run (P=0.02) and time spent running (P=0.01). Bivalirudin/argatroban did not significantly change TETT.
On lung protein analysis, heparin decreased angiogenic signaling compared to controls as demonstrated by decreased activation of VEGFR2 (P=0.03).
Bivalirudin/argatroban did not change activation of VEGFR2; bivalirudin increased endogenous VEGF expression, although not reaching statistical significance.
CONCLUSIONS
Heparin impairs lung growth, exercise tolerance, and angiogenic signaling in an established murine model of CLG following left pneumonectomy. Bivalirudin and argatroban did not impact these outcome measures. This data further supports the use of direct thrombin inhibitors for systemic anticoagulation on ECMO in CDH; DTIs are currently in use at some centers. Based on this work, clinical studies on the impact of heparin and DTIs on CDH outcomes are warranted.
Back to 2022 Abstracts
