Revisiting acute mesenteric ischemia: is there a benefit to leaving the abdomen open?
Jefferson A. Proaño Zamudio, Dias Argandykov, Anthony Gebran, Angela M. Renne, Ander Dorken Gallastegi, Charudutt Paranjape, Stephanie J. Maroney, Haytham Kaafarani, Peter J. Fagenholz, David R. King, George C. Velmahos, John O. Hwabejire
Surgery, Massachusetts General Hospital, Boston, Massachusetts, United States
Objective: Current guidelines advocate for routine use of delayed abdominal closure for planned second-look in patients with acute mesenteric ischemia (AMI) undergoing laparotomy. Few studies have examined this practice. Our goal was to evaluate the effect of delayed abdominal fascial closure on clinical outcomes of patients with AMI. Design: Retrospective cohort study of a national surgical database Setting: American College of Surgeons-National Surgical Quality Improvement Program (NSQIP), years 2013 to 2017. Patients: Patients undergoing emergency laparotomy with a diagnosis of acute mesenteric ischemia. Interventions: Our main exposure was the technique of abdominal wall closure after the index operation. We defined two groups: 1) Delayed fascial closure (DFC): no layers of the abdominal wall closed; 2) Immediate fascial closure (IFC): deep layers of the abdominal wall (fascia) closed, or all layers of the abdominal wall closed. Propensity score matching was performed based on comorbidities, pre-operative, and operative characteristics. Main outcome measures: Primary outcome: in-hospital mortality. Secondary outcomes: in-hospital complications, 30-day mortality Results: 2370 patients underwent laparotomy for AMI in the NSQIP, and 639 (27.0%) received DFC. After propensity score matching, two groups with 415 patients each constituted the final sample. The median age for the matched sample was 68 years (58-77), and 450 (54.2%) were female. In terms of preoperative critical illness, 315 (38.0%) had sepsis, and 365 (44.0%) had septic shock. Bowel resection was performed in 737 (88.8%) of the cases. The DFC group had higher in-hospital mortality (35.9% vs 29.4%, p=0.046), longer hospital stay (13 days vs 10 days, p=0.002), and lower rate of surgical site infection (3.4% vs 8.2%, p=0.003). There were no statistically significant differences in the rate of unplanned reoperation or other postoperative complications. Conclusions: In patients undergoing emergency laparotomy for AMI, DFC is associated with increased in-hospital mortality, increased length of hospital stay, and decreased rate of surgical site infection compared to IFC. Rates of unplanned reoperation were similar between the two techniques. These results do not support a blanket incorporation of temporary abdominal closure into care pathways for AMI. More studies are needed to evaluate which subgroups of AMI patients benefit from delayed abdominal closure for planned second-look laparotomy.
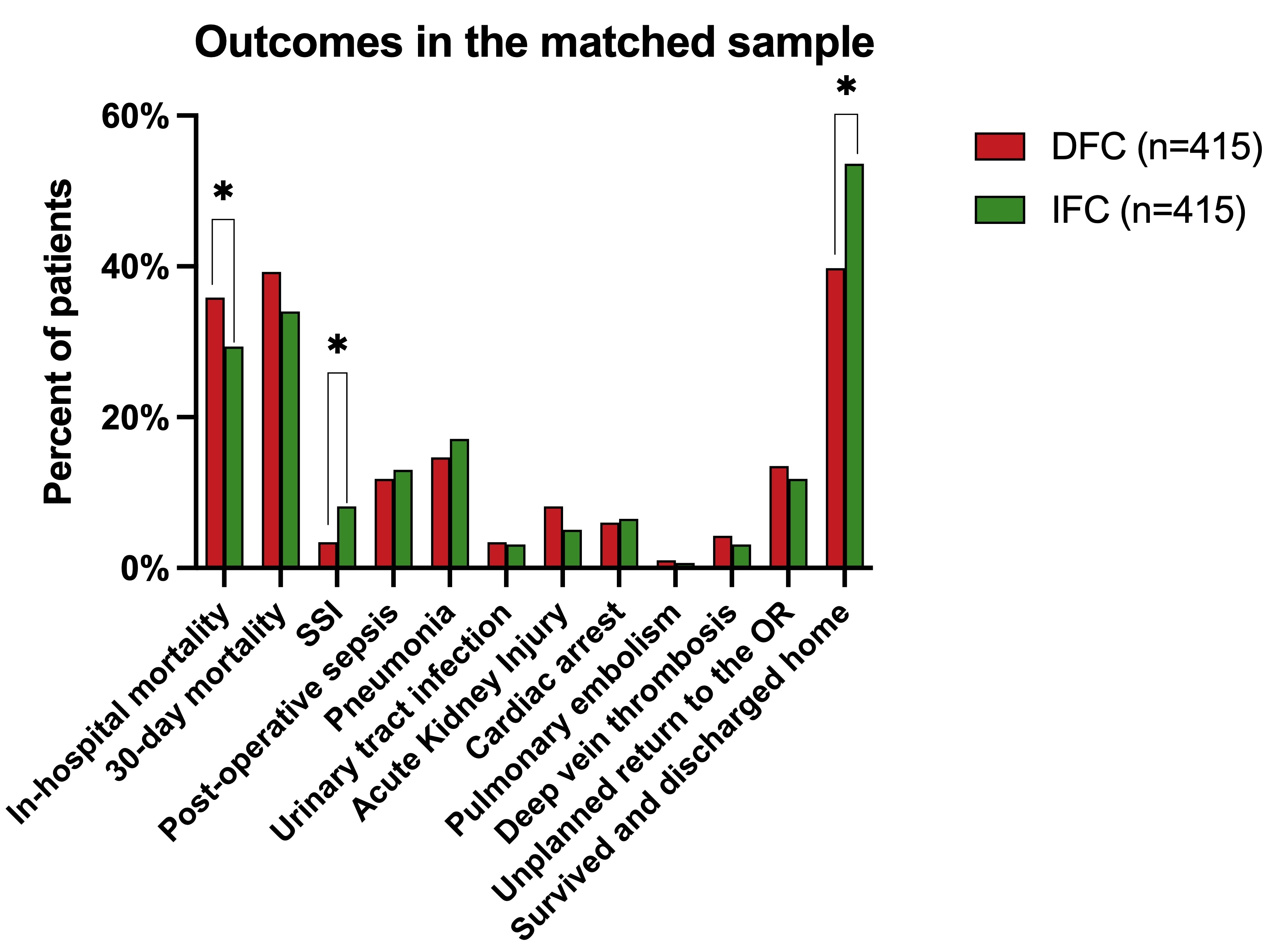
SSI: Surgical Site Infection
OR: Operating Room
Back to 2022 Posters
