Contemporary Postoperative Outcomes for Perforated Appendicitis
Christine Wu, Adam C. Fields, Reza Askari, Stephanie L. Nitzschke
Surgery, Brigham and Women's Hospital, Boston, Massachusetts, United States
Objective
Management of upfront complicated appendicitis can be managed surgically or nonoperatively. While laparoscopic appendectomy is preferred for uncomplicated appendicitis, nonoperative management is common for perforated appendicitis. Recently, immediate operative intervention for perforated appendicitis has become more prevalent; however, historically, a laparoscopic approach has been associated with higher rates of conversion to open and postoperative abscess. We aimed to describe postoperative outcomes for patients with non-perforated and perforated appendicitis stratified by surgical approach.
Design
Retrospective study of surgical intervention for appendicitis identified by 2018-2020 American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Outcomes were compared via chi-squared analysis and analysis of variance tests.
Setting
Hospitals participating in ACS NSQIP.
Patients
Cohort derived from International Classification of Diseases, Tenth Revision codes K35-K37 for appendicitis, followed by current procedural terminology codes organized into 4 procedures: open partial colectomy, laparoscopic partial colectomy, open appendectomy, and laparoscopic appendectomy. 137,397 patients were identified, and variables collected included demographics, preoperative risk factors, wound class, American Society of Anesthesiologists class, and preoperative laboratory values.
Interventions
Not applicable.
Main Outcome Measures
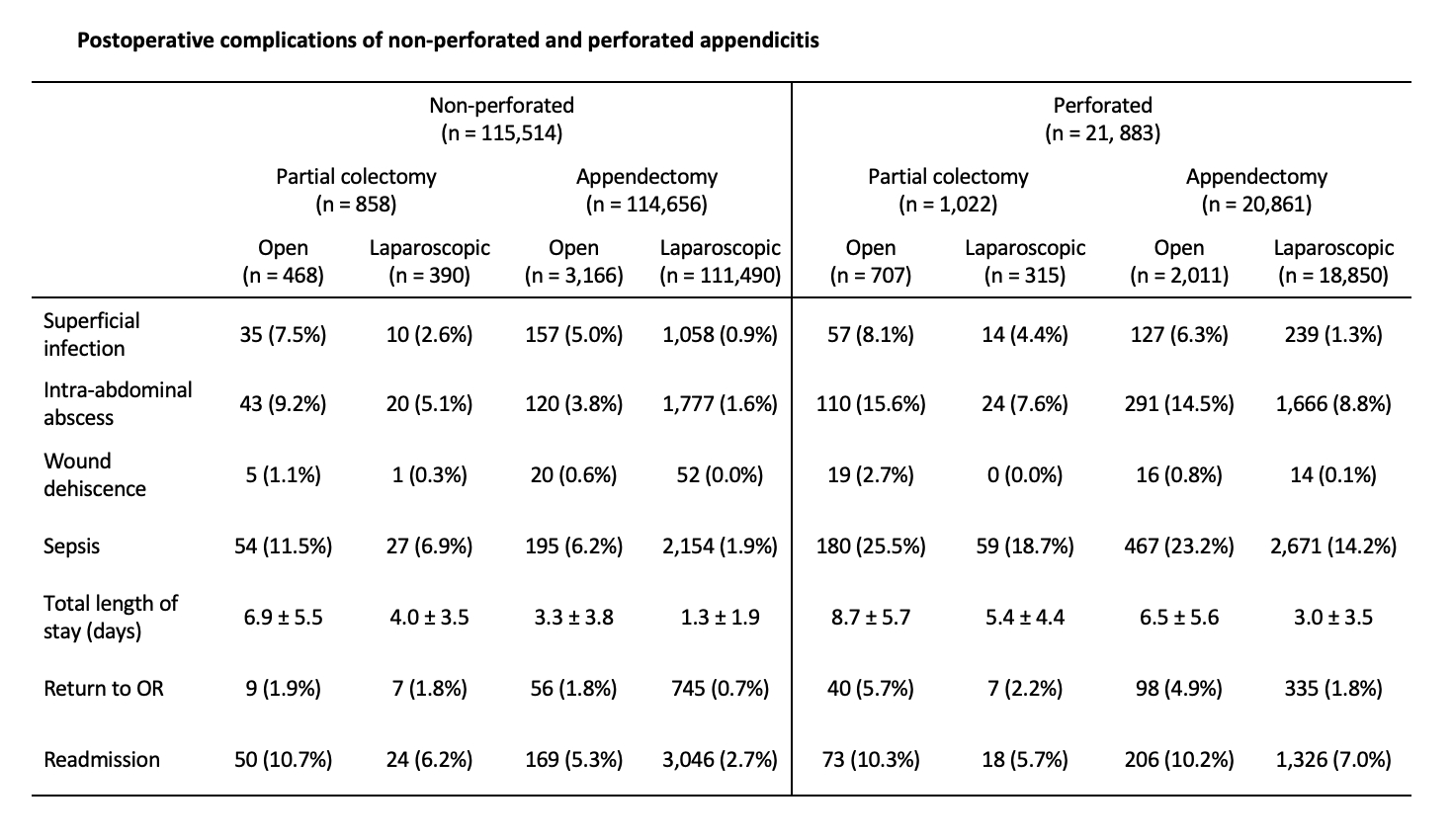
The primary outcomes were length of stay, superficial and deep surgical site infections (SSI), organ space SSI, wound dehiscence, sepsis, return to operating room, and readmission.
Results
From 2018-2020, surgery was performed for 115,514 (84.1%) patients with non-perforated appendicitis and 21,883 (15.9%) patients with perforated appendicitis. Of those with perforated appendicitis, 95.3% underwent appendectomy, with 90.4% via laparoscopy. Superficial SSI, sepsis, reoperation, and length of stay were lowest for laparoscopic appendectomy among all patients. For perforated appendicitis, rates of postoperative intra-abdominal abscess were reduced in those who underwent appendectomy compared to partial colectomy (9.4% vs 13.1%, p < 0.001), as well as laparoscopic compared to open appendectomy (8.8% vs 14.5%, p < 0.001). Wound complications occurred infrequently across all surgical approaches.
Conclusions
Contemporary surgical intervention for perforated appendicitis is predominantly approached laparoscopically and can often be managed by immediate appendectomy alone without cecal involvement. Postoperative complications, including intra-abdominal abscess, occurred less frequently in patients who underwent laparoscopic appendectomy compared to other approaches. Therefore, laparoscopic appendectomy appears to be an effective and safe treatment for perforated appendicitis.
Back to 2022 Posters
