MANAGEMENT AND PREDICTORS OF GASTROESOPHAGEAL REFLUX DISEASE FOLLOWING LAPAROSCOPIC SLEEVE GASTRECTOMY (LSG)
Lyle Suh1, Thuy Duong Doan1, Jeremiah Hyslip1, Nicole Cherng2, Richard Perugini2
1University of Massachusetts Chan Medical School, Worcester, Massachusetts, United States, 2Surgery, UMASS Memorial Medical Center, Worcester, Massachusetts, United States
1. OBJECTIVE
Investigate the utilization of patient-based factors as predictors of GERD status and management following LSG.
2. DESIGN
Retrospective case-control study with post-procedure follow-up.
3. SETTING
Institutional hospital serving the general community.
4. PATIENTS OR OTHER PARTICIPANTS
All patients undergoing longitudinal sleeve gastrectomy (LSG) between March 2019 and July 2020 at UMASS Memorial were included in the study. All patients were in compliance with the 1991 International NIH standards for obesity surgeries. Total: 312 patients
5. INTERVENTION(S)
N.A
6. MAIN OUTCOME MEASURE(S)
1) Prevalence of GERD following LSG
2) Performance of concurrent hiatal hernia (HH) repair during initial LSG procedure
7. RESULTS
Overall GERD prevalence for the entire follow-up cohort was reduced from 37.4% (pre-LSG) to 28.7% (6 months post-LSG). In 51 of 109 (47%) subjects, GERD resolved. However, 24 of 180 (13%) subjects developed de novo GERD. The prevalence of GERD decreased further to 17% by 12 months post-LSG. Pre-procedure UGI findings were not associated with GERD status at follow-up (p = 0.51). In contrast, smoking history increased the risk of GERD post-LSG by 69.6% (p = 0.045). For select patients that received concomitant HH repair with LSG, age, pre-procedure BMI and pre-procedural GERD status were predictors of intraoperative HH repair while pre-procedure UGI performance showed poor prognostic potential (p >0.05). The rate of HH repair increased by 42% with every 10 years increase in patient age (p=0.032) and by 70% with every 5 unit decrease in pre-procedure BMI (p=0.0305). Patients with pre-procedure GERD were more likely to receive HH repair (p = 0.03).
62.2% of patients with GERD post-LSG continued to report GERD at 1-year follow-up, but only 24.4% of these patients underwent post-procedure workups, including pH study, UGI and manometry. However, the degree of GERD symptoms in patients with GERD post-LSG, as quantified based on medications, corresponds to the post-procedure UGI findings (p < 0.010).
8. CONCLUSIONS
This study demonstrated that LSG has beneficial effects for GERD, leading to a significant reduction in prevalence up to at least one year postoperatively. A history of cigarette smoking is associated with presence of GERD following LSG. Age, lower BMI, and preoperative presence of GERD are associated with concurrent HH repair at the time of LSG. Pre-procedure upper GI series did not stratify patients for concurrent HH repair, nor did it predict post-procedure GERD status. Future investigations will focus on expansion of the cohort, examination of postoperative anatomic findings or manometric results as predictive tools, as well as analysis of optimal treatment options for GERD post-LSG.
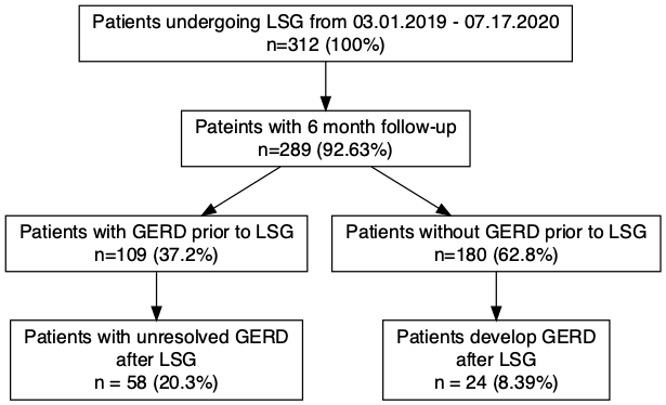
Patient Cohort and GERD status at 6-months follow-up post-LSG
Back to 2022 Posters
