Contemporary Management of Penetrating Diaphragmatic Injury - A Nationwide Analysis
Dias Argandykov, Jefferson A. Proaño Zamudio, Ander Dorken Gallastegi, Anthony Gebran, Angela M. Renne, John O. Hwabejire, Peter J. Fagenholz, David R. King, Haytham Kaafarani, George C. Velmahos, Noelle Saillant
Division of Trauma, Emergency Surgery, and Surgical Critical Care, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts, United States
OBJECTIVE
Traumatic diaphragmatic injuries (DI) often represent both diagnostic and therapeutic challenges. The Eastern Association for the Surgery of Trauma (EAST) has published guidelines on management of DI. Due to paucity of evidence, one of the recommendations encourages conditional management in hemodynamically stable patients with right-sided, penetrating thoracoabdominal injury. In this study using a national database, we aimed to: (1) describe the current management of patients with penetrating DI and (2) evaluate patients who were managed in a delayed fashion.
DESIGN
Retrospective cohort using the American College of Surgeons Trauma Quality Improvement Program (ACS-TQIP) 2016-2019 database
SETTING
Level I-III trauma centers
PATIENTS
Included: Adult trauma patients (≥16 years) with penetrating DI identified by ICD-10-CM codes
Excluded: Patients with no signs of life on arrival, transferred patients, death within 1 hour of admission, hemorrhage control thoracotomy within the first 4 hours
INTERVENTION(S)
Immediate operation (IO) was defined as undergoing a surgical procedure in the thoracoabdominal region within 4 hours of arrival; Delayed operation (DO) was defined as receiving an operative intervention that was offered after 4 hours of arrival.
MAIN OUTCOME MEASURE(S)
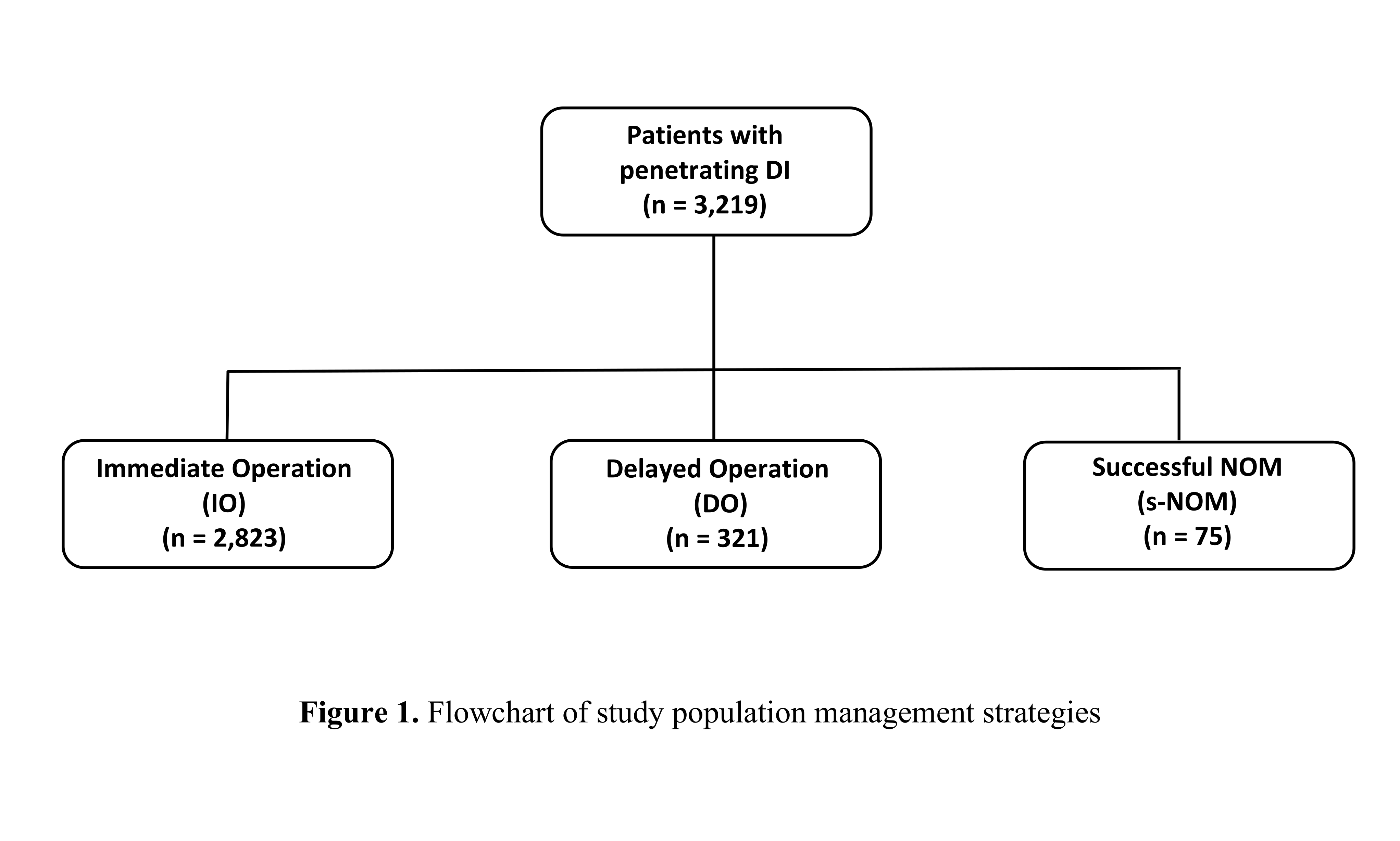
Our primary outcome was the rate of DO and successful nonoperative management (s-NOM), defined as being discharged without any operation (Figure 1). Secondary outcomes included associated injuries and in-hospital complications among s-NOM and DO patients. In the latter group, independent factors associated with DO were evaluated with multivariable logistic regression.
RESULTS
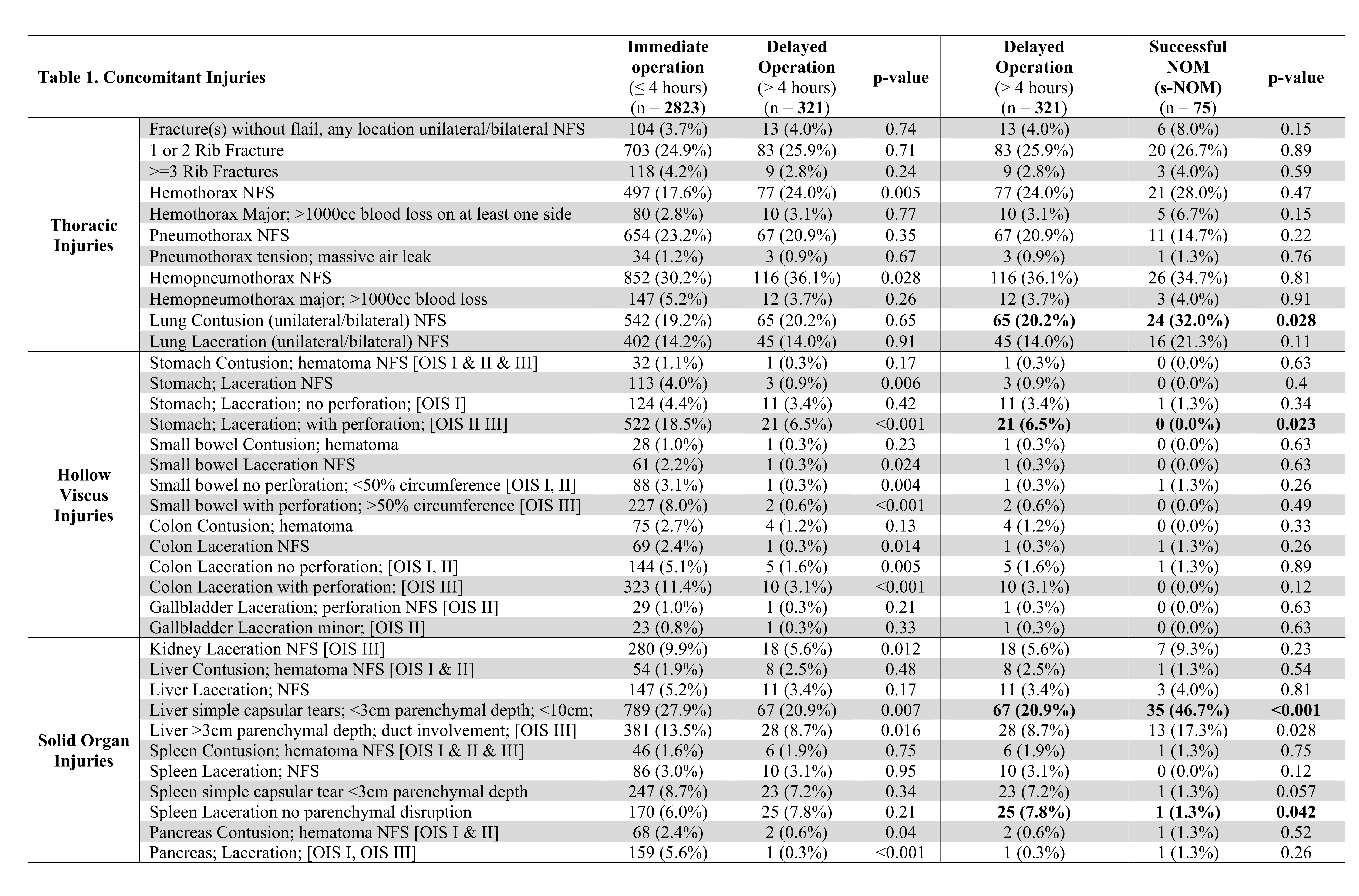
A total of 3,219 patients with penetrating DI were included, of which 2,823 underwent IO (87.7%) and 321 (9.97%) underwent DO. Compared to IO, DO patients had a lower injury severity score and were less likely to have a high-grade DI. Only 75 patients (2.3%) were successfully managed nonoperatively through discharge. s-NOM patients were younger but had a higher injury severity score. Associated injuries were evaluated in patients managed both operatively and nonoperatively (Table 1). The presence of stomach injury was predictive of delayed intervention, while the presence of liver injury corresponding to AAST Grade II was independently associated with s-NOM (aOR = 0.31, 95%CI: 0.18-0.53). Despite delayed intervention, in-hospital complications were not significantly different between s-NOM patients and patients who received DO, although the latter group required longer ICU and hospital length of stay.
CONCLUSIONS
s-NOM of penetrating DI is rarely performed (2.3%) but when done appears to be a safe management strategy when applied to carefully selected patients. The presence of right-sided DI with a surrogate as a liver injury was associated with s-NOM, while stomach injury was a predictor of delayed intervention, and should be considered when selecting patients for operative or nonoperative management.
Back to 2022 Posters
