Impact of Rurality on Geriatric Emergency General Surgery Patients in New Hampshire
Charles P. Burney, Laura Baumann, Heather A. Carlos, Alexandra Briggs
Dartmouth-Hitchcock Medical Center, Windsor, Vermont, United States
Objective
Geriatric patients requiring Emergency General Surgery (EGS) have significant risk of morbidity and mortality. Rural patients face decreased access to care. We sought to characterize the EGS needs and impact of rurality for geriatric residents of New Hampshire (NH).
Design
Retrospective cohort study of the NH Uniform Healthcare Facility Discharge Dataset
Setting
All hospital discharges in NH from 2012-2015
Patients
Patients 65 years-old and older with urgent/emergent admission who underwent one of 7 EGS procedures, grouped by urban or rural county of residence
Main Outcome Measures
Length of stay, cost of index hospitalization, mortality
Results
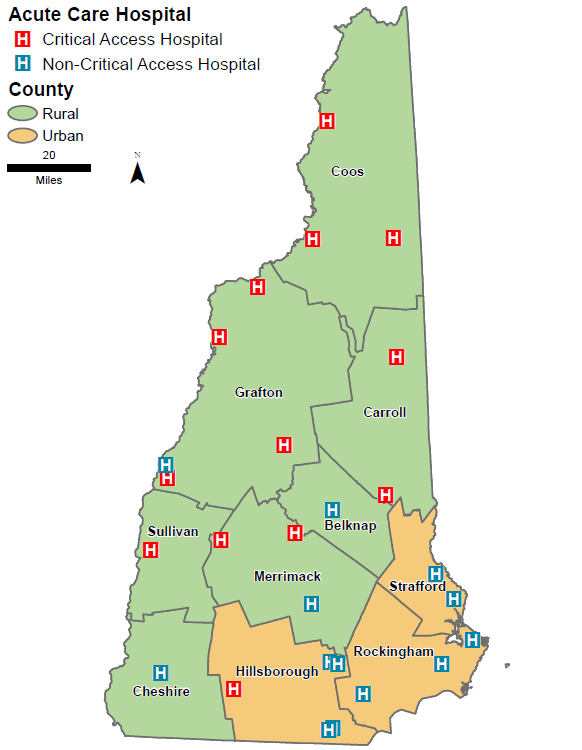
New Hampshire has a total of 26 acute care hospitals (Figure 1) of which 10 (38.5%) are in urban counties and 16 (61.5%) in rural counties. 13 (50.0%) of the hospitals are critical access hospitals (1 urban and 12 rural). Of 2,445 geriatric patient discharges, 40% of patients were from rural counties and were demographically similar to urban patients. Rural patients were more likely to present as a hospital transfer (21% vs 2.6%, p<0.01), receive care at a critical access hospital (24% vs 1.0%, p<0.01), receive care outside their home county (33% vs 13%, p<0.01), and be transferred to another hospital after surgery (count suppressed). Rural and urban patients underwent similar procedures, with similar length of stay, cost of index hospitalization, and mortality.
Conclusions
Rural geriatric patients in NH are more likely to receive care outside of their home county or be transferred to another hospital. Overall costs of care were similar to urban patients but are likely underestimated for rural patients. There was no difference in unadjusted mortality. Further investigation using expanded comorbidity data and geographic granularity to evaluate patterns of care among rural patients is needed.
Back to 2022 Abstracts
