Was it Worth it? A Critical Evaluation of a Novel Outcome Measure in Palliative Surgery
Joshua T. Cohen, Rachel E. Beard, William G. Cioffi, Thomas Miner
Surgery, Brown University, Norwood, Massachusetts, United States
Objective: Outcome measures for palliative surgery remain poorly characterized and limit effective clinical decision making in these complex patients. We explored the usefulness of a specific outcome measure "was it worth it"? in patients following palliative intent operations for advanced malignancy.
Design: Retrospective review of comprehensive longitudinal palliative surgery database
Setting: Academic tertiary-care center
Patients: All patients who underwent palliative-intent operations for advanced cancer from 2005 to 2022 were asked "was it worth it"? within thirty days of operation.
Main outcome measures: Patient satisfaction: "worth it"? (+WIWI) or not "worth it (-WIWI)
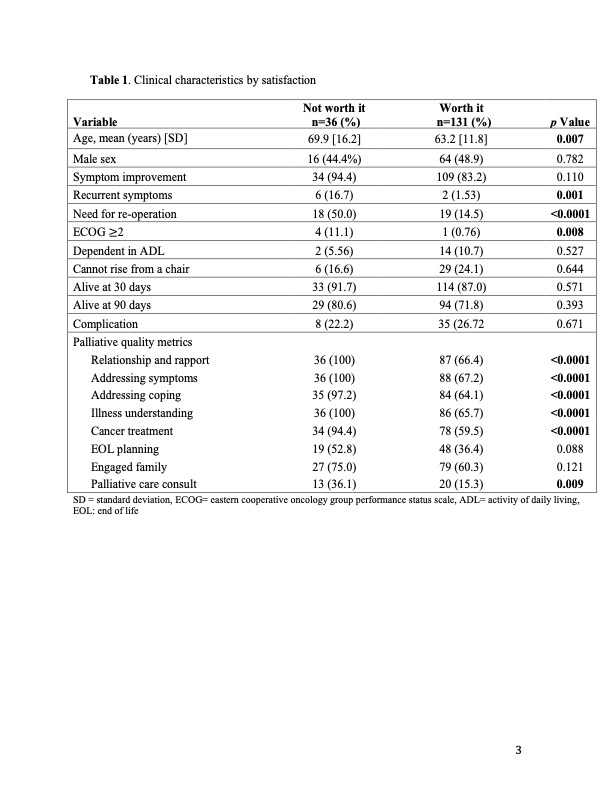
Results: 136 of the168 (82%) of the identified patients reported +WIWI. There was no significant difference in overall (245 vs 227 days p=0.488), recurrence-free (279.5 vs 114 days p=0.110), and re-operation free (226 vs 145 days p=0.346) survival for patients when comparing WIWI reporting. Patient in both cohorts were equally likely to be alive at 30- and 90-days. Patients who reported their surgery -WIWI were older (69.9 vs 63.2 years, p=0.007), more likely to have recurrent symptoms (16.7 vs 1.53%, p=0.001) and to need re-operation (50.0 vs 14.5% p<0.0001). There was no difference in initial post-procedure symptom improvement between groups. After initial response, no -WIWI transitioned to +WIWI. Patients who reported -WIWI were more likely to have met palliative quality metrics, including having developed rapport with the treatment team (100 vs 66.4 %, p <0.001), having their symptoms addressed (100 vs 67.2%, p <0.0001) and coping skills supported (97.2 vs 64.1%, p<0.0001), demonstrating illness understanding (100 vs 65.7%, p<0.0001), undergoing systemic cancer-directed therapy (94.4 vs 59.5%, p<0.0001), and participating in a palliative care consult (26.1 vs 15.2%, p=0.009). Age over 65 (HR 0.25, 95% CI 0.07-0.80, p=0.025), family engagement (HR 6.71, 95% CI 1.49-31.8, p=0.013), and need for re-operation (HR 0.042, 95% CI 0.01-0.16, p<0.0001) were all independently associated with +WIWI patients.
Conclusions: Here we demonstrate that simply asking a patient "was it worth it"? following a palliative intent operation identifies a distinct cohort of patients that traditional outcome measures fail to distinguish, independent of survival and the overall quality of palliative care. Identification of this outcome easily and directly generated from engagement with the patient may help identify those patients who are more likely to have recurrent symptoms and require repeat palliative interventions. Family engagement and durability of an intervention are critical factors in determining patient-specific outcomes following palliative intervention. These data support the individualized care plans made within the context of the goals of the patient and their family.
Back to 2022 Abstracts
