A Multidisciplinary Project to Reduce Post-operative Urinary Tract Infections at a Safety Net Hospital
Spencer Wilson, Pamela Rosenkranz, David McAneny
Surgery, Boston Medical Center, Boston, Massachusetts, United States
Objective: Reduce post-operative urinary tract infections at Boston Medical Center by changing the peri-operative and post-operative practices of urinary catheter insertion, catheter removal, and diagnosis of UTI among healthcare staff.
Design: Chart review of NSQIP post-operative UTIs revealed opportunities to improve adherence to best practices through early foley removal, compliance with existing guidelines, and improving UTI diagnosis. A multidisciplinary quality improvement team was convened and implemented interventions relating to UTI reporting, diagnosis, process improvement, and protocol adherence. The project was evaluated through pre- and post-intervention comparisons of process and outcome data. Intra-operative foley insertion audits were used to determine compliance with proper foley insertion technique.
Setting: Single center safety net urban hospital
Patients: All post-operative patients
Interventions: NSQIP reporters were trained on recognizing UTIs and each UTI case was reviewed in a preventability analysis. Training was provided to providers across surgical specialties on UTI diagnosis and prevention. Training and performance feedback were provided to OR staff on proper foley insertion technique. Foley care kits were developed for patients discharged with foley catheters, along with instructional materials and instructional videos. Foley positioning and UTI prevention awareness materials were distributed throughout surgical floors. Institutional guidelines and best practice advisories were reviewed and revised to promote compliance with foley removal and UTI prevention.
Main Outcome Measure(s): Post-operative UTI rate, foley insertion compliance, provider knowledge, and provider and staff surveys of the training sessions.
Results: Prior to the start of the project, Boston Medical Center was consistently a high outlier among NSQIP institutions for post-operative UTI rates, scoring in the 79th adjusted percentile in 2019. Foley insertion audits revealed low compliance with hand hygiene (62%), sterile insertion (78%), and foley positioning (41%), with only 10% of all foley insertions having overall perfect compliance. Following operating room staff training, compliance rates improved (figure 1), with the rate of overall perfect compliance increasing to 27% (p = 0.047). Following training of residents, scores on a UTI diagnosis knowledge assessment improved from 71% to 81% (p=0.005). The majority of residents and staff "strongly agreed" that training sessions would change their practice (57% and 69%, respectively).
Conclusion: Early process measures from a multidisciplinary quality improvement project to reduce post-operative UTI demonstrate promising improvements in practice. Further efforts directed at staff performance feedback, post-operative adherence to best practices, and patient education are still in progress.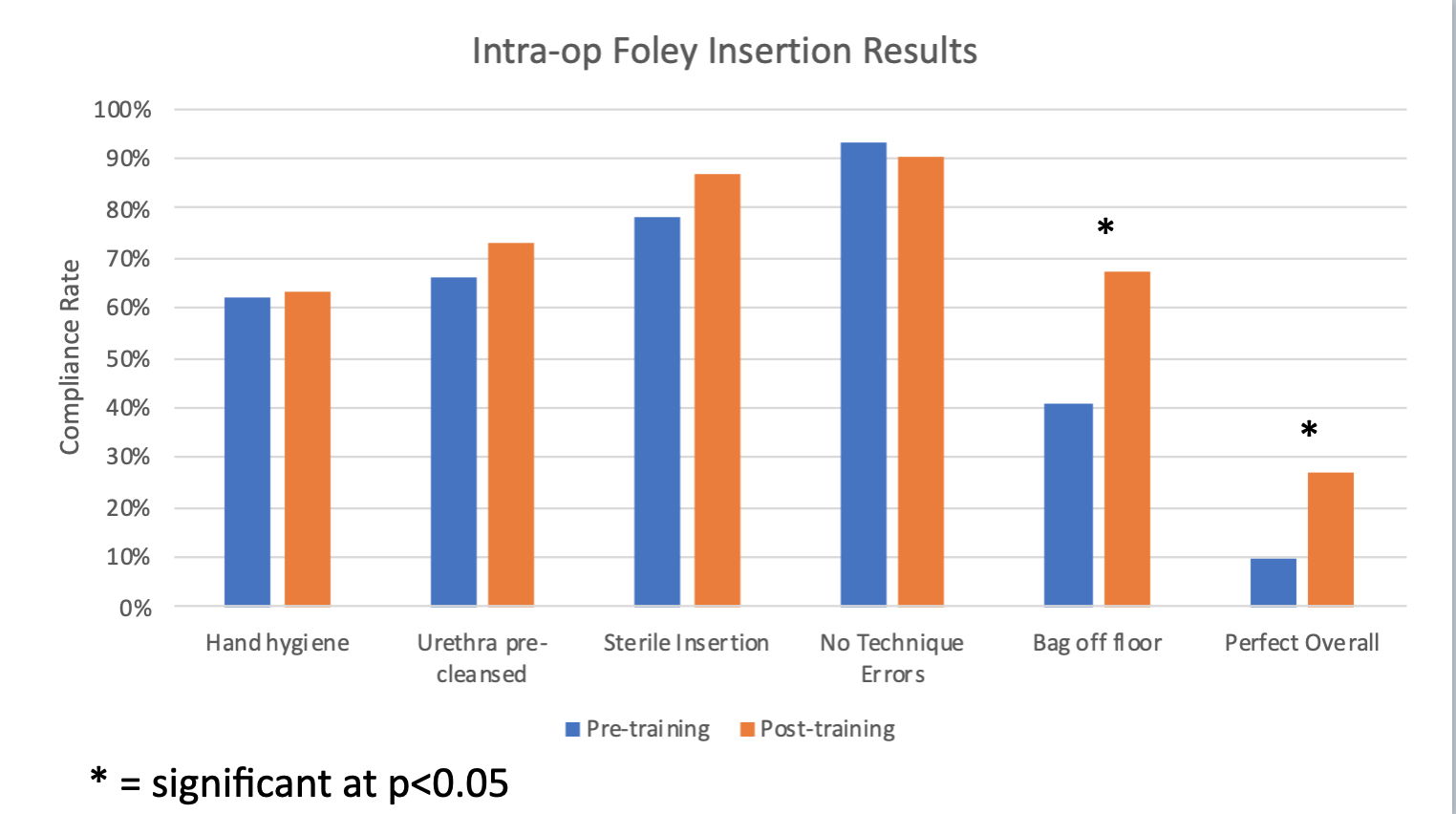
Back to 2021 Abstracts
