Cost-Effectiveness Analysis: Staged versus Nonstaged Techniques for Nipple-Sparing Mastectomy
Yurie Sekigami, Sina Foroutanjazi, Joshua Bloom, Abhishek Chatterjee
Tufts Medical Center, Cambridge, Massachusetts, United States
Objectives: Staged breast reduction prior to nipple-sparing mastectomy (SNSM) has been associated with decreased complications compared to nonstaged nipple-sparing mastectomy (NNSM) and can be helpful in patients with large, ptotic breasts. However, SNSM incurs an additional cost associated with a second surgery. We therefore performed a cost-effectiveness analysis comparing SNSM and NNSM for the treatment or prophylaxis of breast cancer. Design: Cost-effectiveness analysis. Main Outcome Measure(s): Rates of infection, necrosis, wound complications, and explantation for each surgery were obtained from the literature. Procedural costs were calculated from Medicare reimbursement rates. Costs of management of each complication were obtained from literature review. Average utility scores for each health state were previously obtained via visual analog scale, then converted to quality-adjusted life years (QALYs). A decision tree was constructed and incremental cost-effectiveness ratio (ICER) was assessed at $50,000/QALY. Deterministic and probabilistic sensitivity analyses were performed to evaluate the robustness of our findings. Results: SNSM was more costly ($16,520.07 vs $12,994.99) but more effective (26.55 QALY vs 26.2 QALY) than NNSM, resulting in an ICER of $10,062.03/QALY. The Tornado diagram identified that the top three influential parameters were the costs of each surgery and the risk of explantation of NNSM. One-way (deterministic) sensitivity analysis was therefore performed for these three parameters. SNSM became cost-ineffective when its cost was >$27,571.19 or its risk of explantation was >9%. Probabilistic sensitivity analysis was performed using Monte-Carlo simulation which included variations of costs of each surgery, risk of explantation of NNSM, and utility of infection after NNSM. This analysis looking at the variance in the most impactful variables demonstrated that the majority of simulations (99.7%) favored SNSM as the more cost-effective strategy at a willingness to pay of $50,000. Conclusions: Despite its higher cost, SNSM is the more cost-effective strategy compared to NNSM for the treatment or prophylaxis of breast cancer.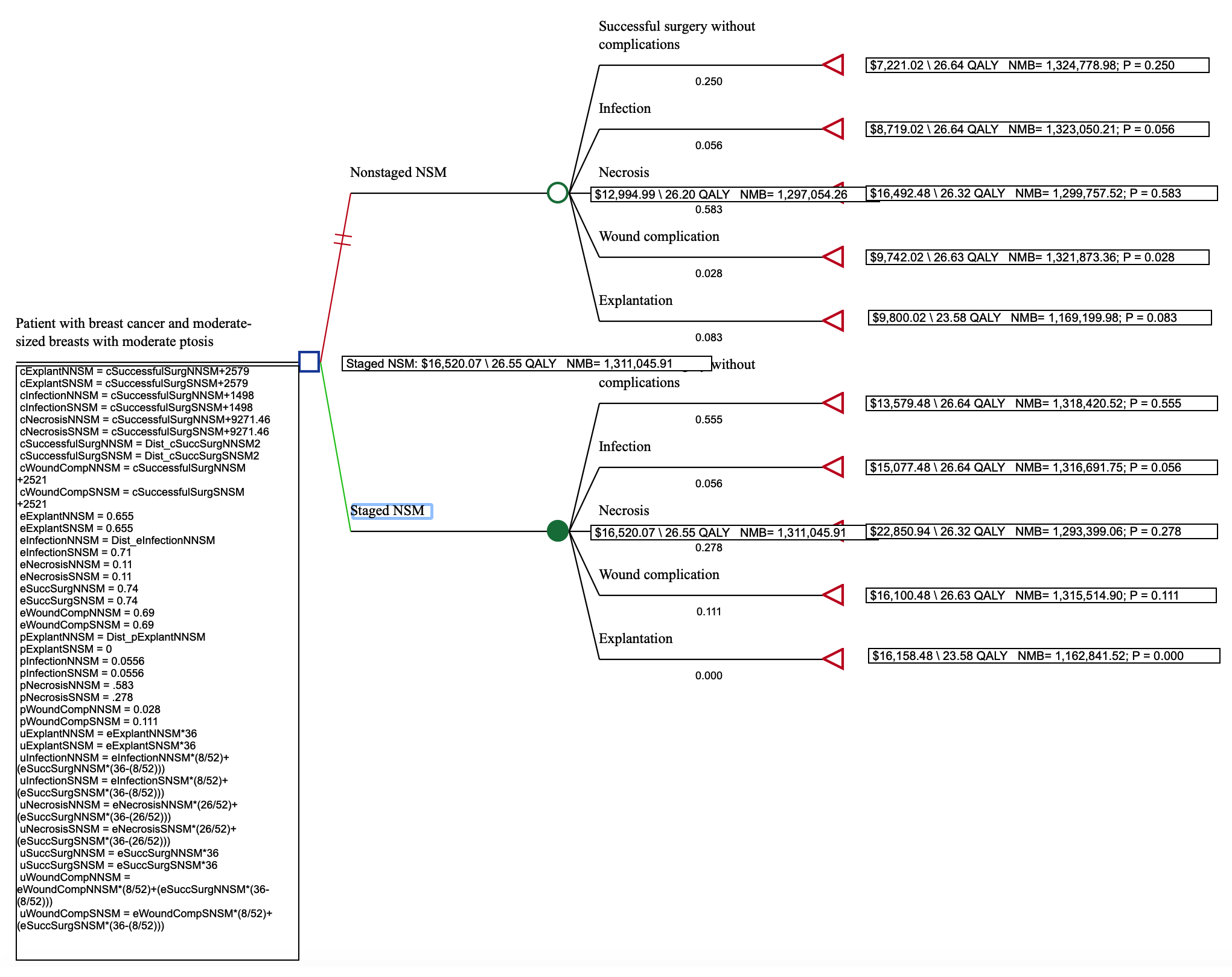
Back to 2021 Abstracts
