How Much is Too Much: Futility During Ultramassive Transfusion in Trauma Patients
Ander Dorken Gallastegi1, Jordan D. Secor1, Lydia Maurer1, Walter H. Dzik2, April E. Mendoza1, Noelle Saillant1, Haytham Kaafarani1, George C. Velmahos1
1Department of Surgery, Massachusetts General Hospital & Harvard Medical School, Boston, Massachusetts, United States, 2Pathology, Massachusetts General Hospital & Harvard Medical School, Boston, Massachusetts, United States
Objectives:
Evaluate the relationship between transfusion volume, transfusion rate, and mortality in trauma patients receiving ultramassive transfusion (UMT).
Hypothesis: In trauma patients receiving UMT, a transfusion threshold exists above which survival is unlikely.
Design:
Retrospective analysis using the American College of Surgeons Trauma Quality Improvement Program (ACS-TQIP) 2010-2018 database.
Setting:
Level I-III trauma centers.
Patients:
Included: Adult trauma patients receiving UMT (≥20 units of red blood cells (RBC) within 24 hours). Excluded: Patients without signs of life on arrival and transferred patients.
Main outcomes measure:
Primary outcome: in-hospital mortality. RBC transfusion volume is recorded at 4 hours and 24 hours after hospital arrival in the ACS-TQIP database. Transfusion rate was calculated as: RBC (units)/time of measurement (4-hr or 24-hr) OR time of death (hr) - whichever came first.
Results
5644 patients were included. A transfusion rate of ≥7 units/hr at 4 hours was associated with a rate-dependent increase in mortality (Figure 1C). Independent predictors of mortality in patients transfused at rates ≥7 units/hr at 4 hours are shown in Table 1. However, a transfusion rate of ≥7 units/hr at 24 hours or time of death was associated with 100% mortality (n=1452 patients) (Figure 1D). A transfusion rate of ≥7 units/hr remained a uniform threshold for mortality among patients who survived at least >4 hours, >8 hours, >12 hours, >16 hours and >20 hours (Figure 2).
Conclusions
Within 4 hours of trauma, RBC transfusion volume and rate are correlated with mortality, but a clear point of futility was not observed. However, beyond 4 hours sustained RBC transfusion rates of ≥7 units/hr are associated with 100% mortality in trauma patients and should warrant consideration of futility.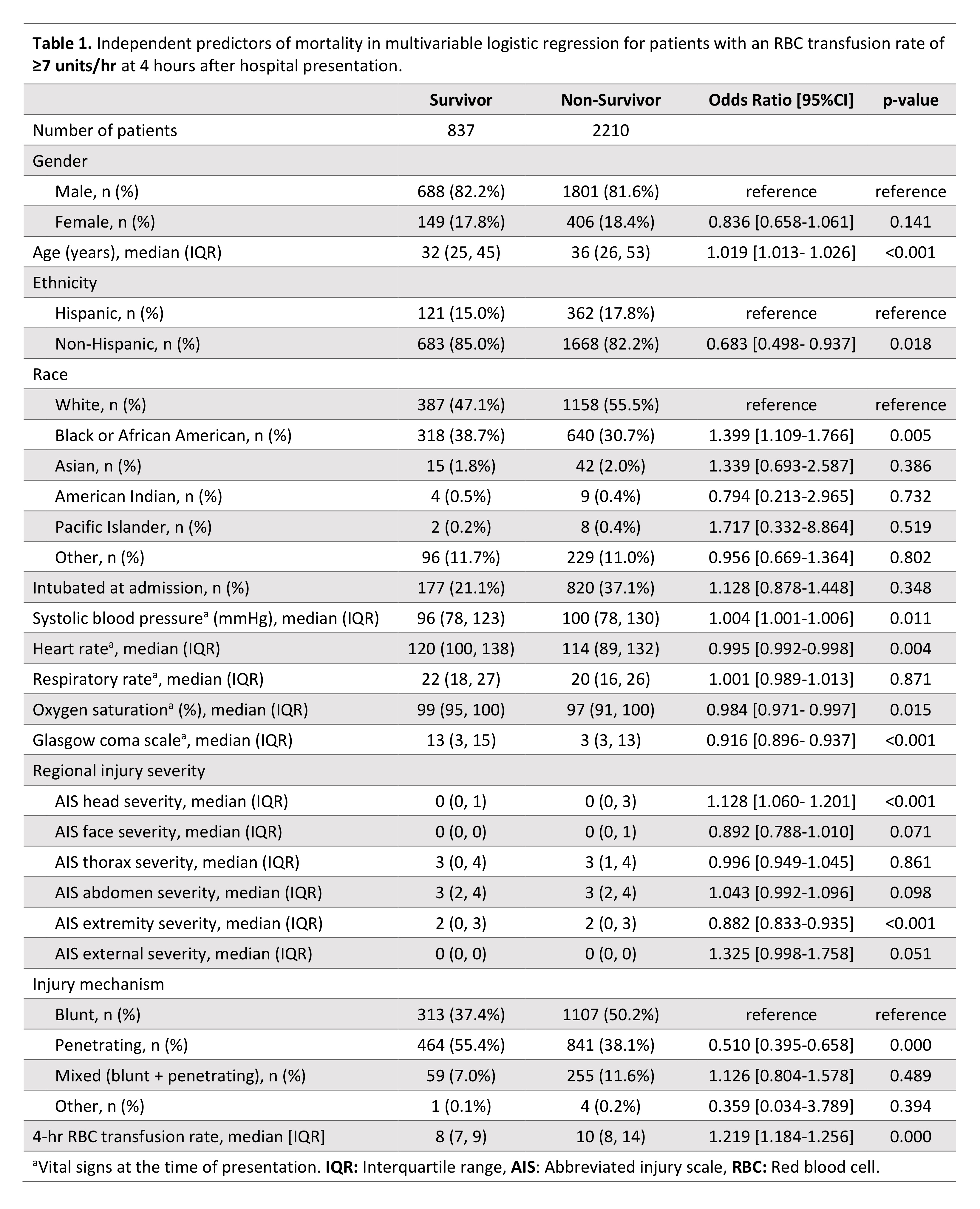


Back to 2021 Abstracts
