Development and Validation of an Esophageal Anastomotic Scorecard to Predict Anastomotic Outcome
Jay Meisner, Ali Kamran, Steven Staffa, David Zurakowski, Somala Mohammed, Russell Jennings, Thomas Hamilton, Benjamin Zendejas
Boston Children"s Hospital, Boston, Massachusetts, United States
Objective: To create an esophageal anastomotic scorecard that predicts anastomotic outcome. Design: Validation Cohort. Setting: Single institution, pediatric referral center. Patients: 74 consecutive pediatric patients (median age 7 months, interquartile range [IQR] 4-20) had an esophageal anastomosis created with a perfusion assessment from 2019-2021. 19 patents were excluded for missing or poor-quality videos. Interventions: Anastomoses underwent near-infrared fluorescence angiography perfusion assessment with intravenous indocyanine green (ICG, SPY-PHI, Stryker). Recorded assessments were thematically analyzed to define qualitative perfusion features to create a perfusion score. Associations between individual perfusion features, perfusion score, degree of anastomotic tension (mild, moderate, severe), and patient-related features with a poor anastomotic outcome were evaluated with uni- and multivariate regression. Significant features were used to create an anastomotic scorecard. Sensitivity and specificity were assessed. Main Outcome Measure: Poor anastomotic outcome (PAO): anastomotic leak or refractory stricture. Results: Median (IQR) follow-up of 5.1 (1.9-13.3) months; 11 (20%) patients experienced a poor anastomotic outcome. Re-operative traction esophageal lengthening procedures (rescue Foker, 15%) were more likely to experience a PAO (50% vs 15% p = 0.042), as well as anastomoses with increased tension (50% severe, 18.2% moderate, 8.7% mild, p=0.027). Based on multivariate analysis, rescue Foker (+1), severe anastomotic tension (+1), lack of arborization (+1), suture line hypoperfusion ≥ twice the expected width (+2), and segmental or global areas of hypoperfusion (+2) comprised the anastomotic scorecard (score range 0-7). A cut-off scorecard score of >2 yielded a sensitivity of 73% and specificity of 86% (AUC 0.85 [95%CI 0.697 to 0.99]) in predicting PAO. Conclusions: Our esophageal anastomotic scorecard with clinical and qualitative perfusion features demonstrates excellent accuracy in predicting a poor anastomotic outcome.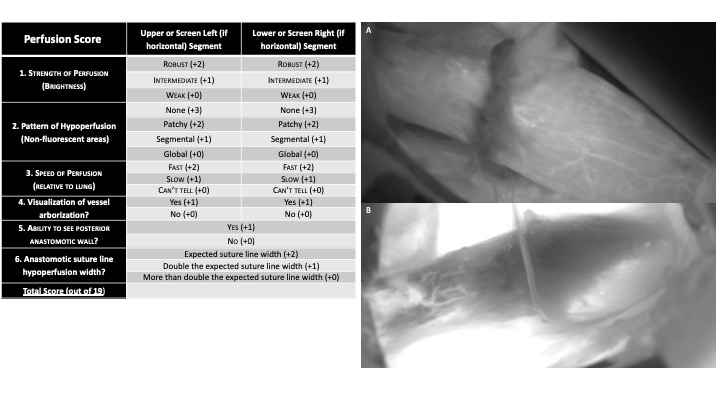
Perfusion Score:
(Right) After completion, each anastomosis underwent a near-infrared fluorescence angiography perfusion assessment with intravenous indocyanine green (ICG) utilizing the SPY-PHI system (portable handheld imager, Stryker). Assessments were recorded and thematically analyzed to define qualitative perfusion features to generate a perfusion score: strength of perfusion (degree of brightness), pattern of hypoperfusion (non-fluorescent areas), speed of perfusion (relative to lung), visualization of vessel arborization, anastomotic suture line hypoperfusion width. Total score is the sum of features 1-4 for both pouches and 5,6 globally.
(A) Example of robust brightness (1), no hypoperfusion (2), presence of arborization on right (4) and expected suture line hypoperfusion width (6)
(B) Example of weak brightness (1), segmental hypoperfusion on right (2), presence of arborization on left (4) and more than double the expected suture line hypoperfusion width (6)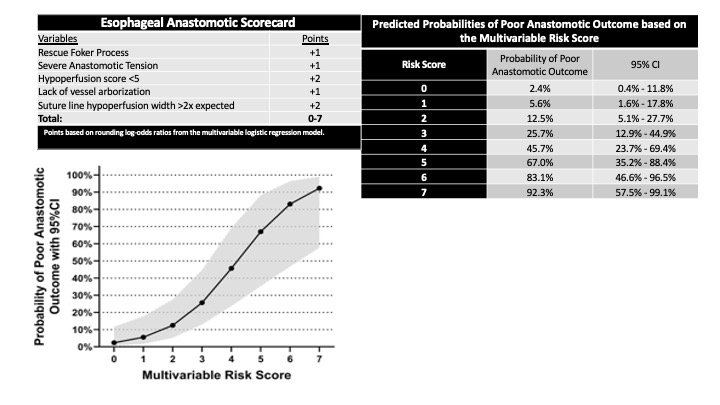
Anastomotic Scorecard
Back to 2021 Abstracts
