A rising tide lifts all boats: combined volume of complex cancer operations protects patient outcomes in a low-volume setting
Susanna W. de Geus, Marianna V. Papageorge, Alison P. Woods, Sing Chau Ng, Andrea Merrill, David McAneny, Jennifer F. Tseng, Teviah E. Sachs
Surgery, Boston Medical Center, Boston, Massachusetts, United States
Objective: Centralization for complex cancer surgery may not always be feasible due to socioeconomic disparities, geographic constraints, or patient preference. The present study investigates how combined volume of complex cancer operations impacts surgical outcomes at hospitals that are low-volume for a specific high-risk cancer operation.
Design: Retrospective cohort study.
Setting: National population-based study.
Patients: Patients who underwent pneumonectomy, esophagectomy, gastrectomy, hepatectomy, pancreatectomy, or proctectomy for malignancy were identified from the National Cancer Data Base (2004-2015). Hospital volume was calculated as operations per year for each focused operation as well as all operations combined. For every operation, three separate cohorts were created: low-volume hospitals (LVH) for both the individual cancer operation and combined complex cancer operative volume, mixed-volume hospital (MVH) with low-volume for the individual cancer operation but high-volume for combined complex cancer operative volume, and high-volume hospitals (HVH) for the specific operation.
Interventions: Pneumonectomy, esophagectomy, gastrectomy, hepatectomy, pancreatectomy, or proctectomy for malignancy
Main outcome measure: 30-day mortality.
Results: In total, 12,463 pneumonectomy, 13,898 esophagectomy, 42,819 gastrectomy,
5,492 hepatectomy, 26,612 pancreatectomy, and 22,199 proctectomy patients were identified. LVH was predictive for 30-day mortality compared to HVH across all studied operations: pneumonectomy (9.5% vs. 7.9%; p=0.0030), esophagectomy (5.6% vs. 3.1%; p<0.0001), gastrectomy (5.4% vs. 2.3%; p<0.0001), hepatectomy (8.1% vs. 5.4%; p=0.0009), pancreatectomy (4.9% vs. 2.4%; p<0.0001), and proctectomy (2.4% vs. 1.6%; p=0.0003). Patients who underwent surgery at MVH and HVH demonstrated similar 30-day mortality across all studied operations: pneumonectomy (6.5% vs. 7.9%; p=0.3083), esophagectomy (2.9% vs. 3.1%; p=0.7207), gastrectomy (2.7% vs. 2.3%; p=0.5034), hepatectomy (4.8% vs. 5.4%; p=0.5106), pancreatectomy (2.8% vs. 2.4%; p=0.4770) and proctectomy (1.4% vs. 1.6%; p=0.6244). All findings were robust on multivariate logistic regression analyses. On sensitivity analyses, the hospital volume for operations in an adjacent anatomic region was the strongest predictor for patients who underwent pancreatectomy.
Conclusion: The results of this study suggest that hospitals that perform sufficient complex cancer operations in total, but are low volume for a specific high-risk cancer operation, demonstrate similar surgical outcomes to centers that are high-volume for the particular operation. These hospitals provide a model for the centralization of complex cancer surgery to improve quality and access to care for patients who do not receive their care at high-volume centers.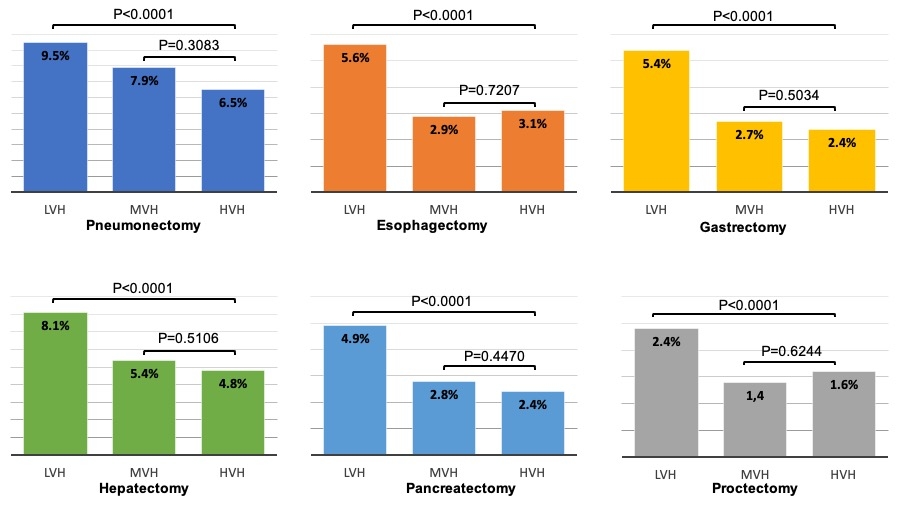
Back to 2021 Abstracts
