POTTER-ICU: An artificial-intelligence interpretable tool to predict need for ICU admission after emergency surgery
Anthony Gebran1, Annita Vapsi2, Lydia Maurer1, Mohamad El Moheb1, Leon Naar1, Sumiran S. Thakur2, Dania Daye3, George C. Velmahos1, Dimitris Bertsimas2, Haytham Kaafarani1
1Division of Trauma, Emergency Surgery, & Surgical Critical Care, Department of Surgery, Massachusetts General Hospital, Boston, Massachusetts, United States, 2Massachusetts Institute of Technology, Boston, Massachusetts, United States, 3Department of Radiology, Massachusetts General Hospital, Boston, Massachusetts, United States
Objective: Delays in admitting high-risk emergency surgery (ES) patients to the ICU result in worse outcomes and increased healthcare costs. We aimed to use interpretable artificial intelligence (AI) technology to create a pre-operative predictor for post-operative ICU need in ES patients.
Design: Retrospective nationwide cohort study.
Setting: 2007-2017 ACS-NSQIP database.
Patients: Adult ES patients.
Main Outcome Measure: Need for post-operative ICU admission, defined as post-operative death or the development of one or more postoperative complication warranting critical care (e.g. unplanned intubation, ventilator requirement ≥48 h, cardiac arrest requiring CPR, and septic shock). Demographics, comorbidities, and laboratory values were included, and a novel, interpretable AI technology called Optimal Classification Trees (OCTs) was leveraged in an 80:20 train:test split to develop the predictive algorithms. An interactive and user-friendly application was created. C-statistics were used to measure performance.
Results: A total of 464,861 patients were included. The mean age was 55 years, 48% were male, and 11% developed severe postoperative complications warranting critical care. Comprehensive OCT algorithms were derived [Figure 1], and the Predictive OpTimal Trees in Emergency Surgery Risk ICU (POTTER-ICU) application was created. The number of questions (i.e. node depths) needed to predict ICU admission ranged from 3 to 12. POTTER-ICU had excellent discrimination for predicting the need for ICU admission (c-statistics: 0.89 train, 0.88 test) [Figure 2].
Conclusions: We recommend POTTER-ICU as an accurate, AI-based tool for predicting severe complications warranting ICU admission after ES. POTTER-ICU can prove useful to triage patients to the ICU and to potentially decrease failure to rescue in ES patients.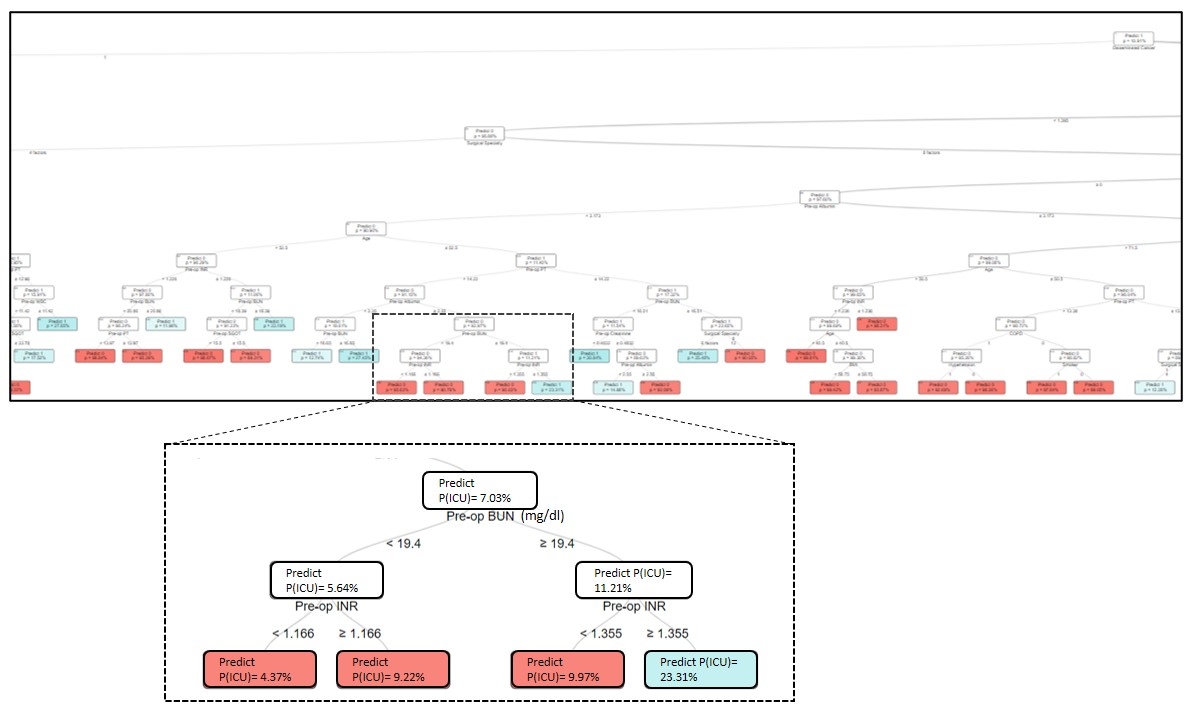 Figure 1: Optimal Classification Trees
Figure 1: Optimal Classification Trees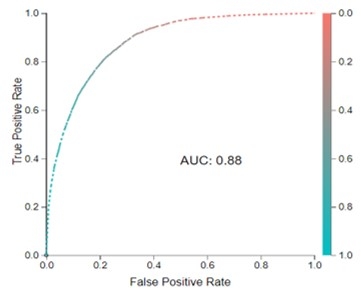
Figure 2: Receiver Operator Characteristic Curve for the Test cohort
Back to 2021 Abstracts
