Frailty Costs: The Economic Impact of Frailty in the Elective Surgical Patient
*Justin Wilkes, *Jessica Evans, *B. Stephen Prato, *Steven Hess, Dougald MacGillivray, Timothy Fitzgerald
Maine Medical Center, Portland, ME
Objective: Frailty is associated with increased morbidity, mortality, and failure-to-rescue. There is little understanding of the economic impact.
Design: A modified version of the Risk Analysis Index was utilized to classify a prospective database of elective surgery patients as not frail (RAI = 0), somewhat frail (RAI = 1-10), or significantly frail (RAI > 11).
Setting: Academic medical center.
Patients: 10,257 elective surgeries (2016-2017).
Interventions: None
Main Outcome Measure: Cost
Results: Frail patients were more likely older (50 vs 65, p < 0.001) and inpatient (19% vs 36%, p < 0.001). On univariate analysis, frail patients were more likely to die (0% vs 0.4%, p < 0.001), have increased LOS (0.8 vs 2.1 days, p < 0.001), higher total cost ($6,934 vs $13,319), and lower net hospital income ($5,447 vs $3,129, p < 0.001). On multivariate analysis, frailty is independently associated with direct cost (OR 2.2, p < 0.001), indirect cost (OR 1.9, < 0.001), total cost (OR 2.2, p < 0.001), and net income (OR 0.8, p < 0.001). In analysis by service line and inpatient versus outpatient status, frailty continues to be associated with increased direct cost, indirect cost, total cost, and decreased hospital income (Figure).
Conclusion: Frailty, independent of age, has a detrimental financial impact on cost and hospital income in the elective surgery patient.
Figure. Total Cost of frail patients (RAI > 11) compared to non-frail patients (odds ratio on logarithmic scale, * = p < 0.05) 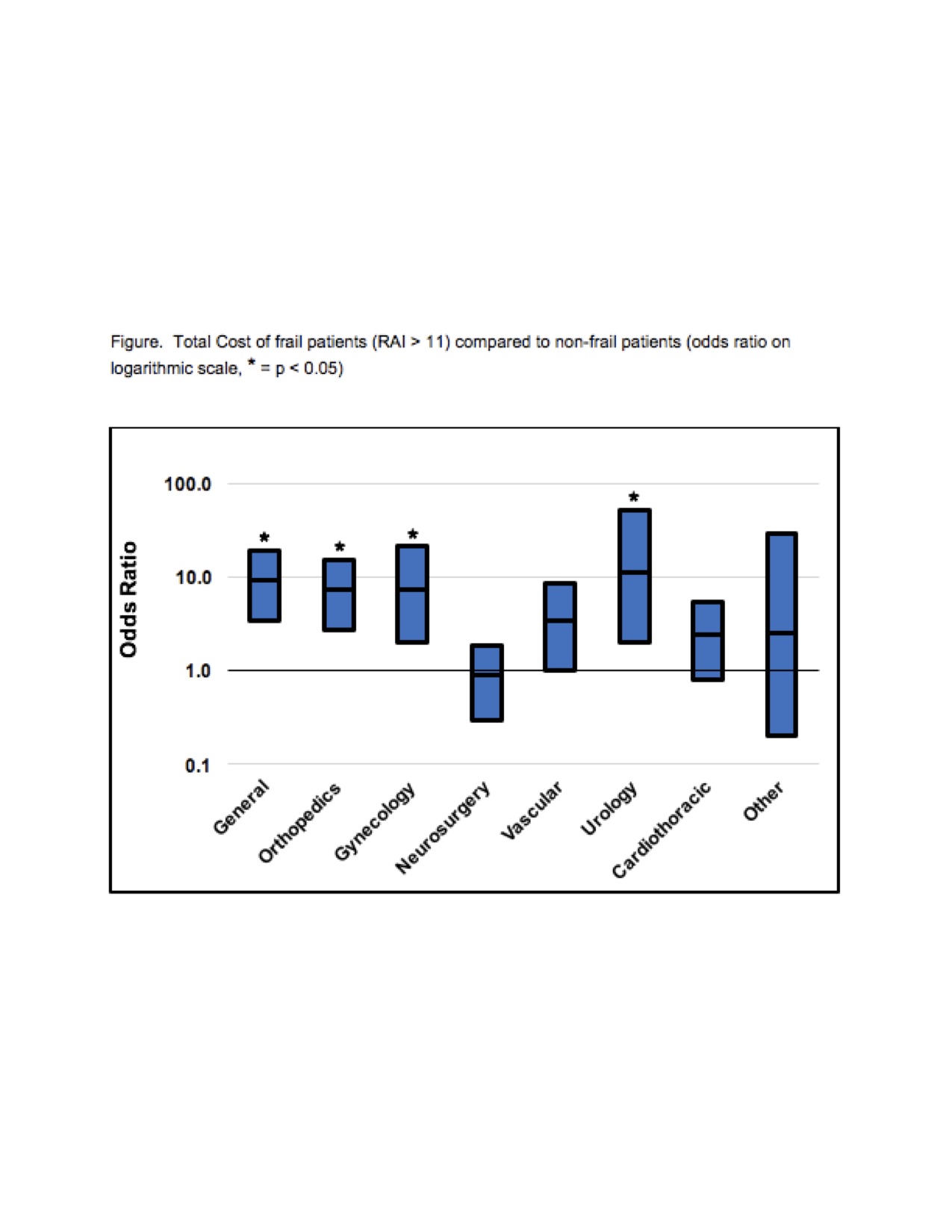
Back to 2018 Program




