Back to 2016 Annual Meeting Posters
Timing of Post-Operative Pneumonia Affects Outcome
*Swathi B Reddy, Kevin M. Schuster, Kimberly A Davis
Yale New Haven Hospital, New Haven, CT
Objective: Postoperative pneumonia (PNA) occurring late ipostoperatively may be distinct from early PNA and require different prevention and treatment strategies. We hypothesized that early and late PNA would have different outcomes.
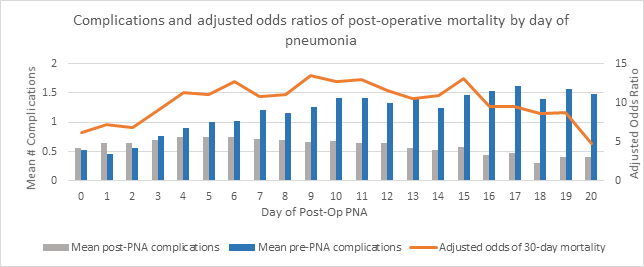
Design: Review of the National Surgical Quality Improvement Program (NSQIP) dataset. Excluded patients had pre-op PNA, were mechanically ventilated preoperatively, were not extubated at surgery or developed ventilator associated PNA. Odds ratios for mortality, adjusting for known risk factors, were calculated for PNA occurring on each day. Early PNA was defined as occurring on postoperative days 2-5 and late on days 8-14 based on mortality trends.
Setting: NSQIP datasets 2005-2014.
Patients: 1,946,532 major elective general or vascular surgery patients.
Interventions: None.
Main Outcome Measures: Mortality and post-PNA length of stay (pLOS). pLOS did not include readmissions for PNA.
Results: 20,024 patients developed PNA with a mortality of 12.1% compared to 0.6% without PNA. Early PNA occurred more often in females and smokers, late PNA in patients with CHF and on steroids (all p<0.05). Early PNA demonstrated lower mortality (10.9% vs. 15.7%, p < 0.001). This was true for the 53.5% of patients without pre-PNA complications (6.5% vs. 9.0%, p=0.002) and those with at least one pre-PNA complication (15.9% vs. 19.4%, p<0.001). pLOS was longer for late-PNA (16.4 days vs. 11.7 days, p <0.0001). This relationship persisted irrespective of pre-PNA complications.
Conclusions: Postoperative PNA impacts patients variably across time independent of comorbidity and other complications, possibly representing several distinct entities. Research and quality improvement efforts should separate early and late PNA.
Back to 2016 Annual Meeting Posters
