Back to 2015 Annual Meeting
Neoadjuvant Radiotherapy for Rectal Cancer Does Not Negatively Affect Short-term Post-Proctectomy Outcomes
*Stefan D Holubar1, *Srinivas J Ivatury1, *Spencer Greaves2, John J Murray1
1Dartmouth-Hitchcock Medical Center, Lebanon, NH;2Medical College of Wisconsin, Milwaukee, WI
Objective: To test the hypothesis that neoadjuvant radiotherapy is associated with increased short-term post-operative outcomes for radical rectal cancer resection.
Design: Retrospective analysis using a large national clinical database (NSQIP).
Setting: NSQIP-participating hospitals in the United States from 2005 - 2010.
Patients: Patients with a diagnosis of rectal cancer (ICD-9 code 154.1) who underwent radical resection.
Interventions: Patients were then stratified into neoadjuvant radiation (within the prior 90-days) vs. none.
Main Outcome Measures: Primary analytic outcome was overall postoperative complications. Secondary endpoints were composite wound complications, length of stay, and death. All endpoints were limited to 30-days post-proctectomy.
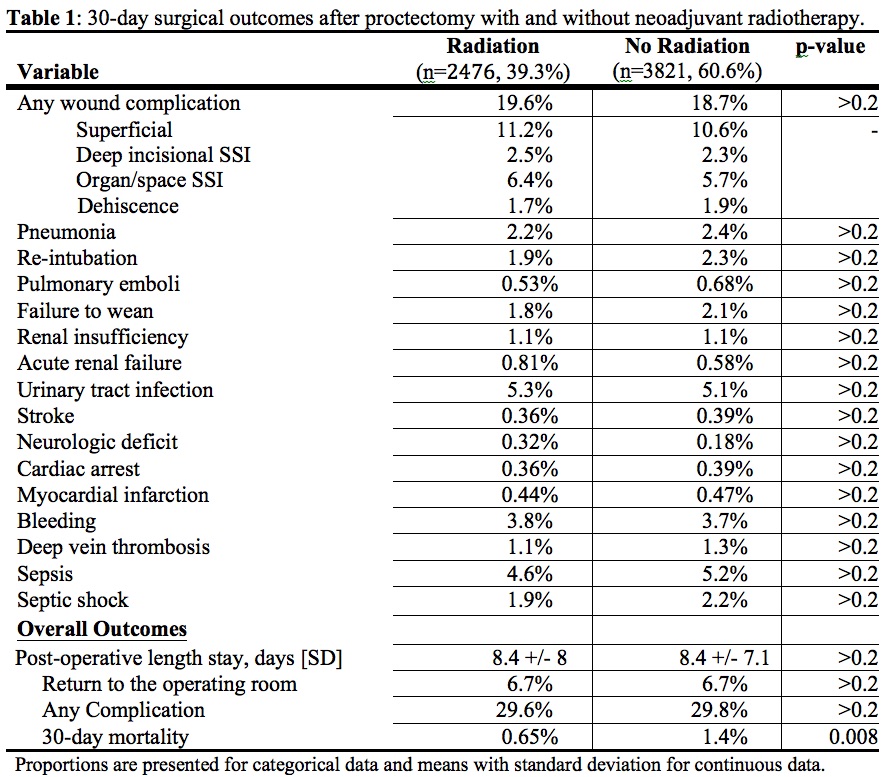
Results: 6,297 patients underwent LAR (49%), APR (34%), CAA (15%), or exenteration (1.4%). Of these, 2,476 (39%) had recent radiotherapy. More irradiated patients, compared to non-irradiated, received chemotherapy within 30 days (15.2% vs. 2.5%, p<0.0001). Irradiated patients were less likely to have laparoscopic surgery (19% vs. 27%, p<0.0001) and less likely to receive a sphincter-preservation (61.8% vs. 67.1%, p<0.0001). Those who had radiation had longer operative times (246 vs. 228 minutes, p<0.0001). There was no difference in overall complications (29% vs. 30%, p=NS), nor wound complications, return to OR, or LOS (Table 1). The mortality rate in the irradiated group was lower (0.6 vs. 1.4%, p=0.008) but this effect was not robust to multivariate analysis including radiation as the primary predictor.
Conclusions: Neoadjuvant therapy for rectal cancer does not negatively affect short-term post-proctectomy outcomes. Given the relatively limited use (<40%) of preoperative radiation, further analysis using the NSQIP-proctectomy module is warranted.
Back to 2015 Annual Meeting
