Back to 2014 Annual Meeting Posters
Feasibility and Benefit of Ex-Vivo Machine Perfusion of Non-Transplantable Deceased Donor Livers
*James Avruch, *Bote Bruinsma, *Pepijn Weeder, *Gautham Sridharan, *Heidi Yeh, *Korkut Uygun, James F Markmann
Massachusetts General Hospital, Boston, MA
Objective: Ex-vivo machine perfusion of livers prior to implantation has been proposed as a potential paradigm shift in DCD transplantation. Our protocol examines machine perfusion of DCD livers compared with cold storage, followed by whole blood reperfusion. The effect of machine perfusion on metabolic activity, graft energy stores, and ischemia-reperfusion injury is examined. We hypothesize that DCD livers which undergo machine perfusion will be more suitable for transplantation and resistant to I/R injury.
Design: Discarded human DCD livers are received with 4-6 hours of cold ischemic time. Livers are randomized to 3 hours of ex-vivo perfusion using the Liver Assist device or 3 further hours of static cold storage; both groups are then reperfused for 3 hours.
Setting: Laboratory
Patients: DCD livers allocated for research.
Interventions: Use of the Liver Assist device for 3 hours of subnormothermic ex-vivo machine perfusion, compared standard cold storage.
Main Outcome Measures: Periodic analyses include measurement of hepatocyte/biliary injury markers, tissue ATP content, liver and bile duct architecture, serum metabolomics, and cytokine analysis.
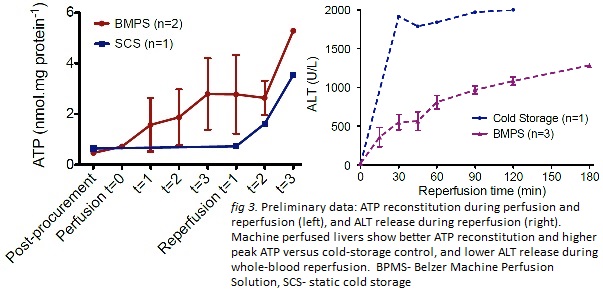
Results: 4 DCD livers have been randomized. The livers in the study group show reconstitution of ATP during machine perfusion and higher peak tissue ATP content compared with cold-stored control. Machine-perfused livers show lower levels of ALT release during reperfusion. (figure 3, attached)
Conclusions: Results show further proof that subnormothermic ex-vivo machine perfusion of DCD livers prior to transplant will expand the organ pool and improve outcomes. Nonanastomotic biliary stricture can be reduced and perhaps eliminated via restoration of tissue ATP prior to implantation.
Back to 2014 Annual Meeting Posters
|
|

