Back to 2014 Annual Meeting Abstracts
Effect of Pre-Admission Beta-Blocker Use on Outcomes in a National Sample of Elderly Americans Undergoing Emergency Abdominal Surgery
*Courtney Collins, *Julie M Flahive, *Fred A Anderson J, Jr, *Heena P Santry
University of Massachusetts, Worcester, MA
Objective
To identify the effect of pre-admission beta-blocker use on outcomes for elderly patients undergoing emergency abdominal surgery (EAS).
Design
Retrospective review of a 5% random sample Medicare claims data including Part D outpatient prescription drug claims (2009-2011)
Setting
US acute care hospitals accepting Medicare patients
Patients
Patients ≥65 undergoing gastric, small intestine, colonic, and hernia operations (by ICD-9 code) during an urgent/emergent hospitalization.
Interventions
Main Outcome Measures
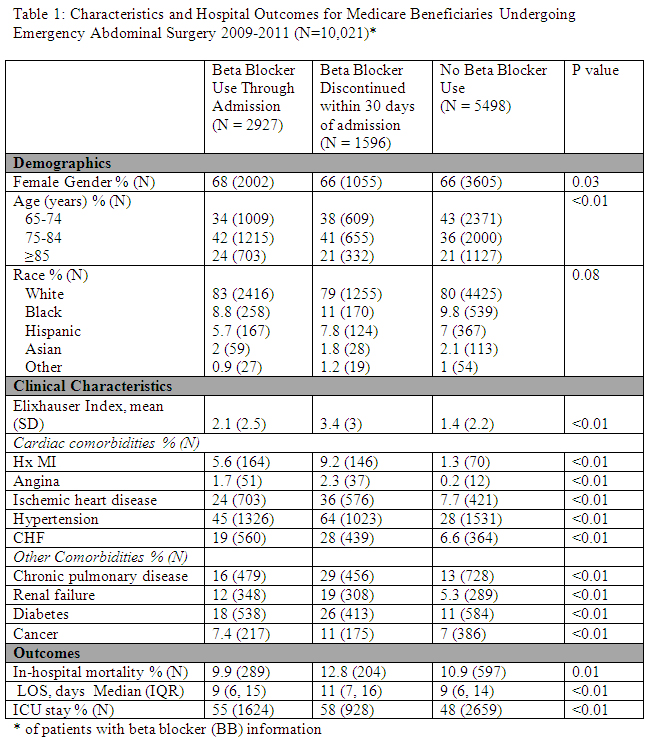
Demographic, clinical, and pre-admission beta-blocker (BB) variables were obtained from Part A/B/D claims. Outcomes (ICU stay, length of stay (LOS), in-hospital mortality) were compared by pre-admission BB usage (none, BB at admission, BB discontinued >30days pre-admission). A multivariable model determined the effect of pre-admission BB use on mortality after EAS.
Results
Of 11,780 EAS patients, 2927(25%) were currently on BB, 1596(14%) had discontinued BBs, and 5498(47%) had never received a BB. Patients who had discontinued BB had higher mortality rates, longer LOS, and higher rates of ICU admission than patients on BBs and those who had never taken a BB(Table 1). In multivariable analyses BB use at the time of admission reduced odds of mortality after EAS by 26% compared to those not on BB(OR 0.74,95% CI 0.63-0.86) while those who had discontinued BB saw no protective effect(OR 0.93,95% CI 0.77-1.1).
Conclusion
Pre-admission BB compliance decreases mortality in elderly patients undergoing emergency abdominal surgery while recently discontinued BBs had no protective effect. Knowledge of patients’ medication adherence in the pre-surgical period may help identify patients at risk of adverse outcomes.
Back to 2014 Annual Meeting Abstracts

