Back to 2014 Annual Meeting Abstracts
Vascularized Flaps for Perineal Wound Reconstruction After Abdominal Perineal Resection for Rectal Cancer: A NSQIP Study
*Stefan D Holubar, *Alex Nourishad, *Gary L. Freed
Dartmouth-Hitchcock Medical Center, Lebanon, NH
Objective:
After abdominoperineal resection (APR) for rectal cancer, patients at high-risk for perineal wound breakdown are selected for perineal wound reconstruction with flaps to reduce surgical site infection (SSI). We hypothesized perineal flap closure compared to primary closure had similar outcomes.
Design:
Retrospective analysis of the 2005 - 2011 American College of Surgeons (ACS) National Surgical Quality Program (NSQIP) Participant User File
Setting:
ACS-NSQIP participating hospitals.
Patients:
Among 13,723 rectal cancer patients, 2,938 (21%) underwent either open- or laparoscopic-APR, or exenteration. Flaps were defined by CPT codes as free or pedicle flaps taken from trunk, lower extremity or gluteus.
Interventions:
Use of flap for perineal reconstruction after APR for rectal cancer.
Main Outcome Measures:
Short-term (30-day) post-operative SSI.
Results:
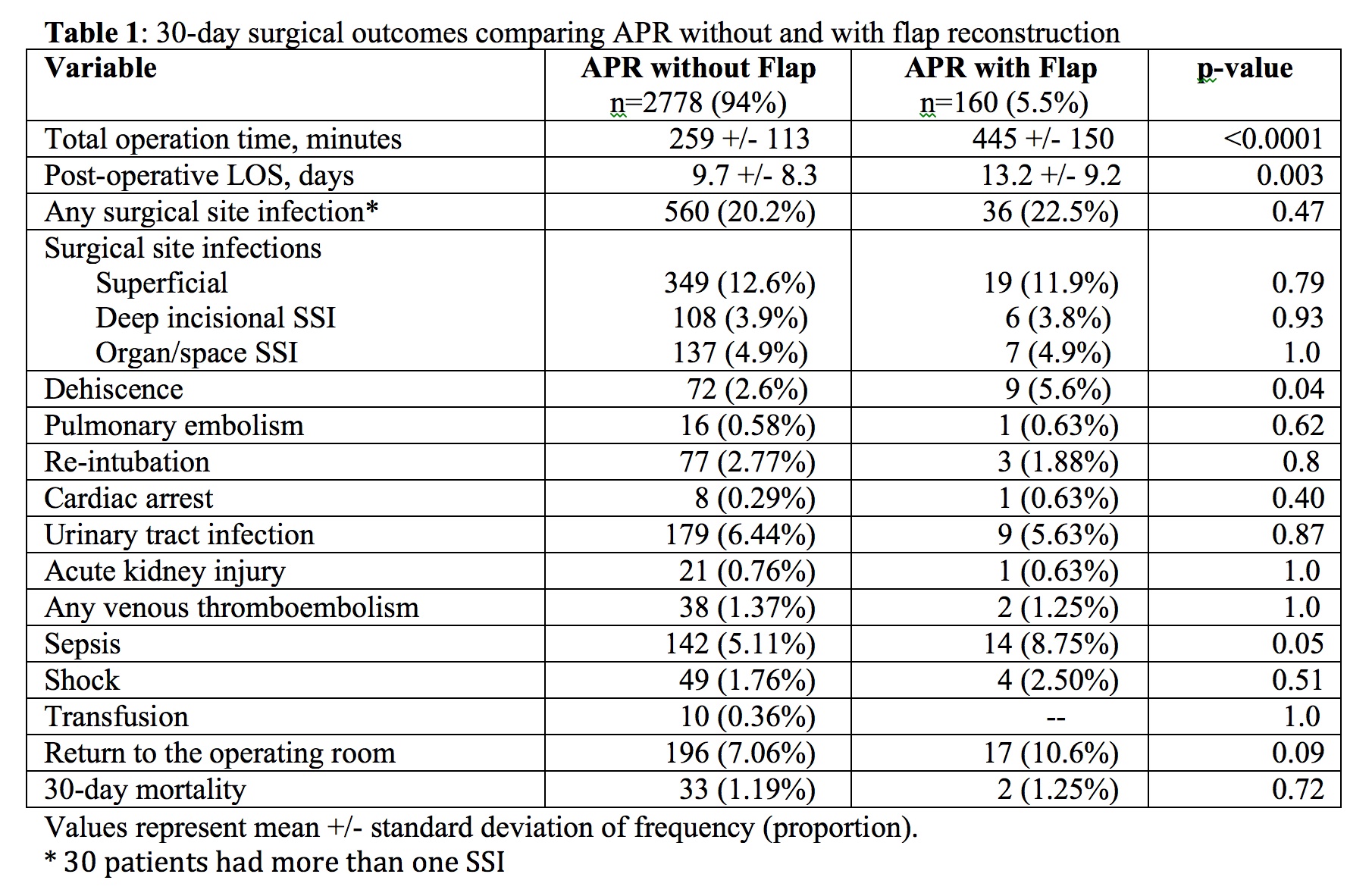
Of 2,938 patients, 160 (5.5%) had a flap closure, and were more likely to be male, younger, have wound infection, weight loss, hypoalbuminemia, anemia, and higher predicted morbidity (27% vs. 24%, p<0.02). Univariate outcomes are shown in Table 1; on multivariate analysis flap was only associated with dehiscence (p=0.02) but not SSI, sepsis, nor LOS. Other independent risk factors for dehiscence were sepsis and weight loss. Flap failure rate was 3.1%; low BMI was the sole risk factor (26.8 vs. 21.9 kg/m2, p=0.0001).
Conclusions:
Primary closure and flap patients had equivalent SSI rate, suggesting flaps prevent SSI. Dehiscence was associated with low BMI, and malnutrition should be aggressively addressed preoperatively for those needing flaps. Further study of patients at highest risk (highest propensity score) to need flap reconstruction, is warranted.
Back to 2014 Annual Meeting Abstracts

